Scene 1 (0s)
[Virtual Presenter] The nervous system is a complex network of interconnected nerve cells that coordinate the body's functions. The central nervous system (CNS) includes the brain and spinal cord, which are responsible for processing information and controlling voluntary movements. The peripheral nervous system (PNS) comprises the nerves that connect the CNS to the rest of the body. The PNS is further divided into two sub-systems: the somatic nervous system (SNS) and the autonomic nervous system (ANS). The SNS controls voluntary movements such as walking, talking, and writing, while the ANS regulates involuntary movements like breathing, heart rate, and digestion. Both systems work together to maintain homeostasis and regulate bodily functions. The autonomic nervous system has two subdivisions: sympathetic and parasympathetic. The sympathetic nervous system promotes relaxation and reduces stress, while the parasympathetic nervous system stimulates activity and increases alertness. The autonomic nervous system plays a crucial role in maintaining overall health and well-being..
Scene 2 (1m 20s)
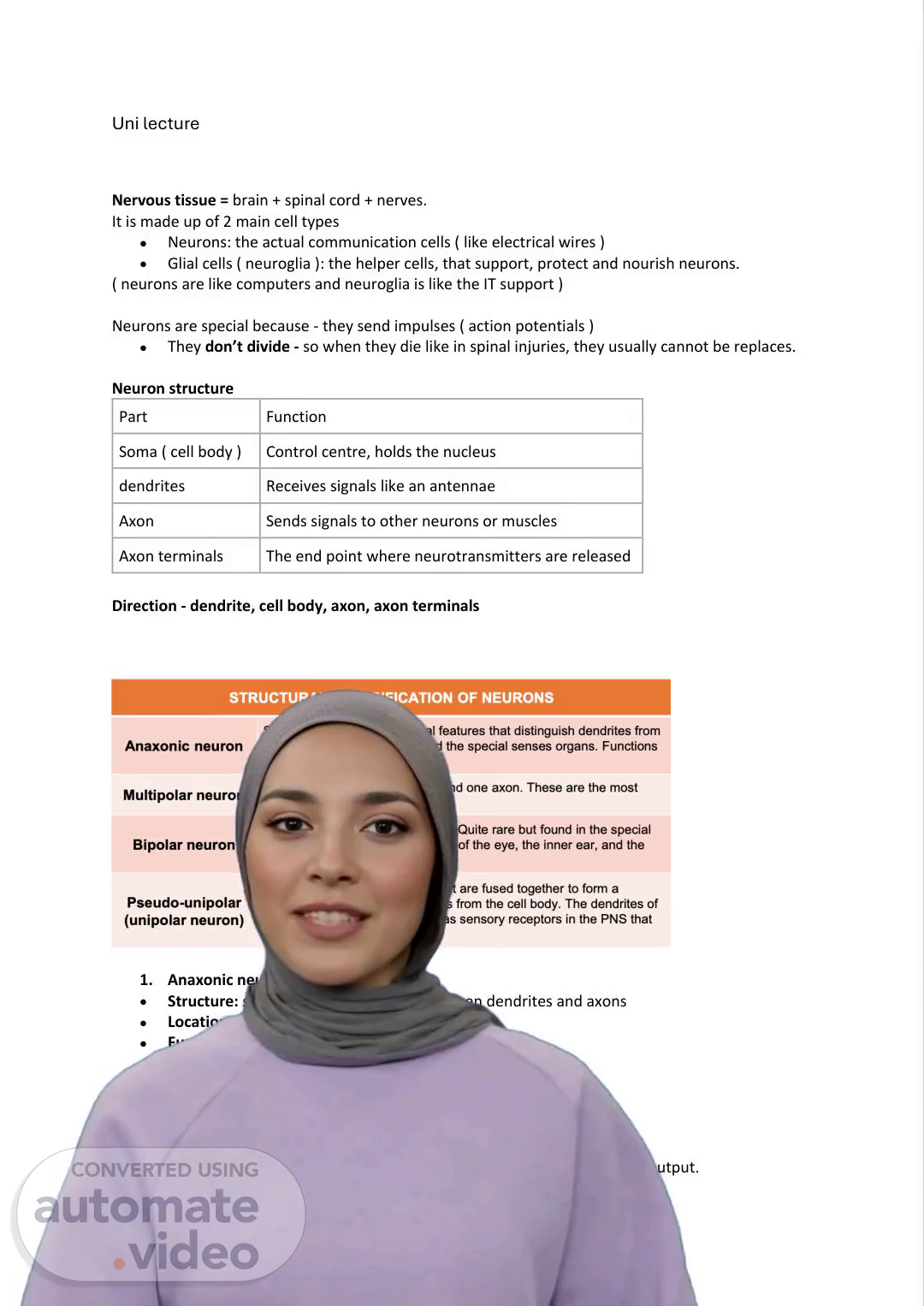
[Audio] The bipolar neuron has a single dendrite and a single axon. The bipolar neuron is located in special sense organs such as the inner eye and the retina of the eye. The bipolar neuron transmits specific sensory information. The pseudo-unipolar neuron has a structure similar to that of the bipolar neuron but it is fused together into one continuous process. The pseudo-unipolar neuron is found in the peripheral nervous system (PNS). The pseudo-unipolar neuron detects sensory stimuli such as touch, pain, and temperature. The myelin sheath is a fatty substance that insulates the axons to speed up signals. The myelination process involves wrapping the axons with myelin. The myelin sheath is produced by the central nervous system (CNS) and the peripheral nervous system (PNS). The nodes of Ranvier are gaps between the myelin segments that help signals jump quickly. The grey matter consists mainly of cell bodies, while the white matter consists mainly of axons due to the presence of myelin. The nervous system is divided into two main parts: the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS includes the brain and spinal cord. The brain is protected by the skull, meninges, and cerebrospinal fluid (CSF). The spinal cord is also protected by the vertebrae. The meninges consist of three layers: the pia mater, arachnoid mater, and dura mater. The CSF cushions the brain and spinal cord and delivers nutrients. The ventricular system is a network of hollow spaces in the CNS that produce CSF. The PNS includes all the nerves outside the brain and spinal cord..
Scene 3 (3m 15s)
[Audio] The spinal nerves consist of 31 pairs that act as a conduit between the central nervous system (CNS) and the rest of the body. These nerves are made up of two main components: dorsal roots and ventral roots. Dorsal roots receive sensory input from the environment and transmit it to the spinal cord. Ventral roots carry motor signals from the spinal cord to muscles and glands. A nerve has a layered structure similar to a cable, comprising multiple layers including endoneurium, perineurium, and epineurium. Understanding the anatomy of the nervous system is necessary to comprehend its physiological functions. The nervous system's primary functions include gathering sensory input, integrating processed information, and producing motor outputs. The system can be divided into sensory and motor divisions, each performing distinct tasks. The sensory division receives signals from the CNS and transmits them to other parts of the body. The motor division sends signals from the CNS to muscles and glands throughout the body. Within the motor division, there are subcategories like somatic and autonomic, which control different types of muscles and organs. Somatic division controls voluntary movements, while autonomic division regulates involuntary actions such as digestion, heart rate, and respiration. The brain processes information using distinct lobes, each responsible for specific functions like movement, sensation, and cognition. The visual system uses about 70% of all sensory receptors to detect light and transmit signals to the brain for interpretation. Comprehending the nervous system's intricate workings is essential to appreciate its complex mechanisms and functions..
Scene 4 (5m 14s)
[Audio] The auditory and vestibular systems work together to enable us to perceive our environment through sound and balance. The auditory system is responsible for allowing us to hear, which is crucial for speech recognition. The vestibular system senses head movements, position, and balance to maintain equilibrium. The ear is divided into three regions: the external, middle, and internal ears. The external ear collects sound waves and directs them towards the eardrum, where they are converted into mechanical vibrations by the tympanic membrane. The middle ear amplifies these vibrations using the three tiny bones, known as ossicles. The internal ear processes these vibrations further, converting them into neural signals that are transmitted to the brain. This process involves several key steps, including the capture of sound waves by the auricle, the transmission of these waves through the external auditory canal and eardrum, and the conversion of these waves into mechanical vibrations by the tympanic membrane. These vibrations are then amplified by the ossicles and processed by the cochlea, which converts them into neural signals. The vestibular apparatus, located in the inner ear, detects changes in head movement and position, helping to maintain balance and equilibrium. This includes sensing both static and dynamic movements, such as standing still versus walking or turning. The vestibular apparatus consists of two main components: the semicircular ducts, which detect rotational movement, and the utricle and saccule, which detect linear movement. Together, these structures provide the brain with information about head movement, enabling it to maintain balance and equilibrium..
Scene 5 (7m 6s)
[Audio] The cardiac cycle is made up of two main parts: systole and diastole. Systole refers to the phase where the heart contracts and pushes blood out, while diastole is the relaxation phase where the heart fills with blood. The sequence of events is atria contract - ventricles contract - whole heart relaxes. This process ensures that blood flows from high pressure areas to low pressure areas, using one-way valves to prevent backflow. The heart also has specialized cells called cardiomyocytes, which include conducting cells and contractile cells. Conducting cells act as the heart's pacemaker, generating automatic electrical signals that trigger the heartbeat. They are responsible for setting the heart rate and initiating the electrical signal that spreads across the atria, causing them to contract. In contrast, contractile cells are responsible for squeezing blood out of the heart, responding to the electrical signal from conducting cells. The conduction system, consisting of the SA node, AV node, AV bundle, and Purkinje fibers, plays a crucial role in coordinating the heartbeat by transmitting the electrical signal through the heart in a precise manner. The SA node acts as the natural pacemaker, setting the heart rate, while the AV node introduces a slight delay to ensure that the atria have finished contracting before the ventricles start. The AV bundle and Purkinje fibers then transmit the signal through the ventricles, allowing for coordinated contraction. The result is efficient blood flow, where blood is pushed upward into arteries from both the atria and ventricles..
Scene 6 (8m 51s)
[Audio] The sinoatrial node acts as the heart's pacemaker, generating electrical impulses that stimulate the heart muscle to contract. The electrical impulses are generated by the movement of ions across the cell membrane, specifically the movement of sodium and potassium ions. The sinoatrial node has a unique property: it does not require any external stimulus to generate electrical impulses. Instead, it relies on the gradual depolarization of its membrane potential, caused by the slow leakage of sodium ions into the cell. As the membrane potential becomes more positive, the cell eventually reaches a threshold and fires an action potential, which initiates the heartbeat. The action potential is triggered by the opening of calcium channels, allowing rapid depolarization to occur. The potassium ions then leave the cell, causing repolarization and resetting the cell's membrane potential back to its original state. The process repeats itself, creating a continuous cycle of electrical activity that drives the heartbeat. The atria are stimulated to contract by the electrical impulse, and the ventricles follow suit. The intercalated discs and desmosomes play a crucial role in enabling fast communication and strong adhesion between cardiac cells, allowing them to work together seamlessly. The plateau phase allows for a longer contraction period, ensuring that the ventricles can pump blood efficiently. The sinoatrial node's ability to generate electrical impulses without external stimulation makes it an essential component of the heart's functioning..
Scene 7 (10m 35s)
[Audio] The electrocardiogram, or ECG, is a graphical representation of the electrical activity of the heart. It displays three main waves: the P wave, the QRS complex, and the T wave. These waves correspond to specific events in the heartbeat process. The P wave represents the atria contracting and pushing blood into the ventricles. The QRS complex indicates the ventricles contracting and pumping blood out to the lungs and body. The T wave signifies the ventricles relaxing and filling with blood again. A flatline on the ECG indicates a lack of electrical activity, resulting in no contraction and no blood flow. Understanding the structure and function of the heart is essential for grasping the importance of circulation. Circulation is vital for maintaining life, as it ensures the continuous movement of blood throughout the body. This movement follows a natural gradient from high to low blood pressure. There are two primary circulatory pathways: pulmonary circulation and systemic circulation. Pulmonary circulation involves transporting blood to the lungs to obtain oxygen and expel carbon dioxide. Systemic circulation, on the other hand, delivers oxygen and nutrients to the body while collecting waste products. Both systems rely on the heart's pumping action to facilitate this exchange. In pulmonary circulation, deoxygenated blood from the body enters the right atrium via the vena cava. From there, it passes through the tricuspid valve into the right ventricle, which contracts and sends the blood through the pulmonary semilunar valve into the pulmonary trunk. The blood then branches into left and right pulmonary arteries, traveling to the lungs where oxygenation occurs. Finally, oxygen-rich blood returns to the left atrium via pulmonary veins. Understanding the intricacies of these circulatory pathways is crucial for appreciating the complexity of the cardiovascular system..
Scene 8 (12m 46s)
[Audio] The key points of this slide are the two types of circulations: pulmonary and systemic. Pulmonary circulation involves the transport of oxygen-poor blood from the right side of the heart to the lungs, where it becomes oxygen-rich, and then returns to the left side of the heart. Systemic circulation, on the other hand, involves the delivery of oxygen-rich blood to the body's tissues and the removal of waste products. Both circulations involve the movement of blood through arteries, capillaries, and veins, and both play critical roles in maintaining overall health. The body regulates blood pressure through various mechanisms, including the baroreceptor reflex and the renin-angiotensin-aldosterone system. These systems work together to maintain homeostasis and ensure that blood pressure remains within a healthy range. Understanding these concepts is essential for appreciating how the cardiovascular system functions and how it responds to changes in the body's needs..
Scene 9 (13m 49s)
[Audio] The cardiovascular control centre plays a crucial role in regulating blood pressure and blood volume. This hormonal system kicks in over hours or days, responding to changes in blood pressure and volume. When kidney detects low blood pressure or low blood volume, it releases renin, triggering a cascade that ultimately leads to vasoconstriction and retention of water and salt. This results in increased blood pressure and stabilized blood volume. The cardiovascular control centre, located in the medulla oblongata, has three main paths that regulate blood pressure: the cardioaccelerator centre, the cardioinhibitor centre, and the vasomotor centre. These centres work together to increase heart rate and strength through the sympathetic nervous system, slow down the heart through the parasympathetic nervous system, and control blood vessel diameter through the vasomotor centre. Vasoconstriction causes blood vessels to narrow, increasing blood pressure, while vasodilation causes them to widen, decreasing blood pressure. Cardiac output and blood pressure are closely linked, with cardiac output determined by stroke volume and heart rate. Blood pressure is also influenced by vessel diameter, with increased cardiac output and vasoconstriction leading to higher blood pressure. Haemostasis is the process by which the body stops bleeding, involving platelets and red blood cells working together to form a clot. This process occurs quickly and locally at the site of injury, with platelets releasing chemicals to initiate clotting and red blood cells helping to stabilize the clot..
Scene 10 (15m 37s)
[Audio] The body's response to injury is complex and multifaceted. The process of stopping bleeding involves several distinct stages. These stages include vascular spasm, platelet plug formation, and blood coagulation. Vascular spasm causes blood vessels to constrict and slow down blood flow. Platelet plug formation is a positive feedback loop where platelets adhere to exposed collagen, aggregate, and form a temporary patch. Blood coagulation is the final stage, where the clot becomes permanent due to the activation of prothrombinase and conversion of prothrombin to thrombin. Intrinsic and extrinsic pathways converge to a common pathway, involving cofactors such as vitamin K and calcium. Fibrinolysis is the process of breaking down clots, which is essential for preventing embolism. Understanding these stages helps appreciate how the body regulates bleeding and maintains homeostasis. The key to distinguishing between primary and secondary haemostasis lies in recognizing that primary haemostasis forms a temporary patch, while secondary haemostasis creates a permanent clot. Fibrinolysis serves as the 'clean-up crew', responsible for dissolving clots once they are no longer needed. Grasping these concepts enables students to better comprehend the intricate mechanisms underlying human physiology..
Scene 11 (17m 7s)
[Audio] The respiratory system has two main parts: the upper respiratory tract and the lower respiratory tract. The upper respiratory tract includes the nose, pharynx, and larynx, while the lower respiratory tract consists of the trachea, bronchi, and lungs. These different parts work together to facilitate the exchange of gases between the environment and the bloodstream. The most basic function of the respiratory system is to provide oxygen to the body and remove carbon dioxide. This process occurs through the exchange of gases between the lungs and the bloodstream. The respiratory system is made up of various organs and structures that work together to achieve this function. The organs of the respiratory system include the nose, pharynx, larynx, trachea, bronchi, and lungs, all of which play a crucial role in facilitating gas exchange. The blind-ended alveoli in the lungs are responsible for exchanging oxygen and carbon dioxide. The structure of the respiratory system allows it to function efficiently, enabling us to breathe and maintain our bodily functions..
Scene 12 (18m 21s)
[Audio] The blood supply to the lungs comes from two main sources: the bronchial circulation and the pulmonary circulation. The bronchial circulation provides oxygen-rich blood at high pressure to the structures of the airway and the visceral pleura. The pulmonary circulation takes blood from the right side of the heart, which is weak and has no oxygen, and makes it oxygen-rich by pumping it back throughout the body. This process involves the pulmonary arteries and bronchial arteries, which bring blood into the lungs and then the pulmonary veins and bronchial veins that take the oxygen-rich blood out of the lungs. The conducting zone, located at the beginning of the airway, plays a crucial role in warming, moistening, and filtering the air we breathe. It includes the nose and nasal turbinates, the pharynx, the larynx, and the trachea. These structures work together to prepare the air for gas exchange in the lungs. The pulmonary circulation is responsible for delivering oxygen-rich blood to the body's tissues. The pulmonary veins carry this oxygen-rich blood from the lungs to the left side of the heart. From there, the blood is pumped throughout the body by the left ventricle. The pulmonary circulation also helps to remove carbon dioxide from the body by carrying it away from the lungs through the pulmonary veins and bronchial veins. The conducting zone is essential for gas exchange because it warms, humidifies, and filters the air we breathe. Without it, the air would be too cold and dry to support life. The structures within the conducting zone work together to ensure that the air reaches the lungs in optimal condition. The air is then exchanged with the blood in the lungs, allowing the body to obtain the oxygen it needs. The process of gas exchange is critical for maintaining life..
Scene 13 (20m 18s)
[Audio] The airway system starts with the connection of the larynx to the bronchi. This connection is crucial as it allows air to pass through the lungs. The bronchi are lined with mucus and cilia, which work together to create a self-cleaning mechanism. Cilia move the mucus upwards towards the throat, where it can be swallowed or coughed out. This process is known as the mucociliary escalator. In smokers, the damage caused by smoking leads to the death of cilia, resulting in increased mucus production and a need for manual coughing to clear the mucus. The respiratory zone is where gas exchange occurs, involving the transfer of oxygen into the blood and carbon dioxide removal from the blood. This zone includes the respiratory bronchioles, alveolar ducts, alveolar sacs, and alveoli. The respiratory bronchioles have a thin layer of smooth muscles and elastic fibers, allowing them to control airflow and facilitate gas exchange. They branch off into alveolar ducts, which then lead to the alveolar sacs and finally to the alveoli. The alveoli are the site of gas exchange, where oxygen diffuses into the blood and carbon dioxide diffuses out. The structure of the alveoli is such that they allow for efficient gas exchange, making them essential for the functioning of the respiratory system..
Scene 14 (21m 45s)
[Audio] The respiratory system is a complex network of organs and tissues that plays a crucial role in the process of respiration. One of the key components of this system are the lungs, where the exchange of gases takes place. The alveoli are tiny air sacs that form the functional unit of the lungs. They are responsible for the exchange of gases between the lungs and the blood. Within the lungs, there are over two million alveolar ducts that carry air to the alveolar sacs. These sacs contain hundreds of millions of alveoli, giving your lungs a vast surface area for gas exchange. The alveoli are also connected by tiny holes called alveolar pores, which allow for equalization of pressure and facilitate air flow. These pores also aid in the diffusion of gases between neighboring alveoli. The alveoli are made up of three major types of cells: type 1 alveolar cells, type 2 alveolar cells, and alveolar macrophages. Type 1 cells are thin, squamous epithelial cells that make up the structure of the alveolus. On the other hand, type 2 cells are cuboidal epithelial cells that secrete pulmonary surfactant and are more numerous than type 1 cells, but they cover less surface area. Alveolar macrophages, also known as the "big eaters," are mobile scavengers of the immune system that engulf foreign bodies that make it into the lung tissue. The respiratory membrane, comprised of the endothelium of the surrounding capillary and the thin epithelium of a single alveolus, is only 0.5 micrometers thick. This allows for the exchange of gases through simple diffusion, with oxygen being picked up by the blood for transport and carbon dioxide being released into the air of the alveoli to be expelled. In summary, the alveoli are essential for efficient gas exchange in the lungs. Their unique structure and various types of cells allow for the exchange of gases between the lungs and the blood. The complex respiratory membrane provides a thin barrier for gas diffusion, allowing for respiration to take place..
Scene 15 (24m 3s)
[Audio] The transport of blood gases involves several key mechanisms. Firstly, the capacity of haemoglobin to bind oxygen is crucial. Haemoglobin has a high affinity for oxygen, allowing it to carry approximately 98% of the oxygen in the blood. This oxygen is then chemically combined with haemoglobin to form oxyhaemoglobin. Another critical aspect is the solubility of gases in blood plasma. Oxygen dissolves in plasma at a concentration of around 2%. Carbon dioxide, on the other hand, is transported in three different forms. Firstly, it is chemically combined with haemoglobin to form carbaminohaemoglobin, which accounts for 20-30% of the total CO2. Secondly, CO2 is chemically modified as bicarbonate ions, making up around 60-70% of the dissolved CO2. Finally, some CO2 is chemically modified further as carbonic acid, but this is less significant. The transport of blood gases is closely linked to the mechanics of breathing. Breathing refers to the physical movement of air in and out of the lungs, bringing in oxygen and removing carbon dioxide. Respiration, however, is the biological process of gas exchange, where oxygen is moved into cells and carbon dioxide is removed from cells. There are four main processes involved in respiration: pulmonary ventilation, external respiration, respiratory gas transport, and internal respiration. Pulmonary ventilation is the physical act of breathing in and out, driven by pressure differences between the lungs and atmosphere. External respiration occurs at the interface between the air and blood, where oxygen diffuses into the blood and carbon dioxide diffuses out. Respiratory gas transport involves the movement of gases through the bloodstream, carrying oxygen from the lungs to tissues and carbon dioxide from tissues to the lungs. Internal respiration occurs within the cells themselves, where oxygen is used to produce energy and carbon dioxide is produced as a waste product. Overall, the transport of blood gases is a complex process involving multiple mechanisms and processes. Understanding these mechanisms is essential for appreciating how the respiratory system functions..
Scene 16 (26m 35s)
[Audio] The human body has two main organs responsible for gas exchange: the lungs and the liver. The lungs are primarily responsible for exchanging oxygen and carbon dioxide through the process of respiration. The liver performs a similar function but on a smaller scale. Both organs have specific structures and functions that enable them to facilitate gas exchange. The lungs contain numerous tiny air sacs called alveoli, where gas exchange takes place. The liver contains bile ducts and sinusoids, which facilitate the exchange of substances. The structure and function of both organs are critical to maintaining overall health and well-being. The efficiency of gas exchange is vital for proper bodily functions..
Scene 17 (27m 23s)
[Audio] The human body produces a special substance called pulmonary surfactant, which is similar to soap. This substance reduces surface tension in the alveoli, making it easier to breathe. Pulmonary surfactant spreads between water molecules, decreasing the tight grip they have on each other, thus lowering surface tension. This results in the alveoli expanding more easily and being less likely to collapse. Additionally, pulmonary surfactant affects lung compliance. Lung compliance refers to the ease with which the lungs can expand during inhalation. Two factors contribute to lung compliance: elastic fibers in lung tissue and surface tension in the alveoli. Elastic fibers provide structure and help the lungs expand and recoil. However, if surface tension is too high, the lungs may become stiff and difficult to inflate. On the other hand, if surface tension is too low, the lungs may not spring back well after inflation. Air resistance plays a significant role in breathing. Airway resistance occurs when air travels through the airways, causing friction due to the rubbing of air molecules against the walls of the airways. High airway resistance makes it more difficult to breathe, while low airway resistance allows for smoother airflow. Several factors influence airway resistance, including airway radius, turbulent air flow, and dirty or polluted air. Maintaining acid-base balance is crucial for overall health, as even small changes in blood pH can have severe consequences. The body tightly regulates blood pH levels between 7.35 and 7.45, and any deviation from this range can lead to serious health issues..
Scene 18 (29m 19s)
[Audio] The bicarbonate buffer system plays a crucial role in maintaining blood pH stability. This system utilizes three key chemicals: carbon dioxide, water, and bicarbonate. Carbonic acid (H2CO3) is a weak acid, while bicarbonate (HCO3-) acts as a weak base. Under normal conditions, when blood becomes too acidic, bicarbonate binds additional hydrogen ions to form carbonic acid, which is then converted into CO2 and exhaled. Conversely, when blood becomes too basic, carbonic acid releases hydrogen ions, thereby reducing the pH level back to normal. Bicarbonate serves as the primary buffer of extracellular fluid, including blood plasma. Both the lungs and kidneys regulate blood pH, although they operate at different speeds. The lungs rapidly eliminate excess acid through exhalation, whereas the kidneys gradually remove excess acid or base through urine production. An increase in CO2 levels leads to a drop in pH, causing blood to become more acidic. On the other hand, a decrease in CO2 levels results in an increase in pH, leading to blood becoming more basic. Respiratory disturbances, such as hypoventilation or lung diseases, can lead to respiratory acidosis, characterized by an increase in H+ ions and a subsequent drop in pH. Conversely, hyperventilation can result in respiratory alkalosis, marked by a decrease in H+ ions and an increase in pH. Metabolic factors, like excessive acid or base loss, can also disrupt pH balance. Kidney failure or diarrhea can lead to metabolic acidosis, while vomiting or antacid overuse can cause metabolic alkalosis. The human body has a remarkable capacity for homeostasis compensation, where one system compensates for the failure of another. For instance, if the lungs fail to regulate pH, the kidneys will adjust breathing rates to compensate. Similarly, if the kidneys fail to remove excess acid, the lungs will increase breathing rates to expel CO2 and restore pH balance. The regulation of respiration is primarily controlled by CO2 levels rather than O2. Hypercapnia, or elevated CO2 levels, triggers an increase in H+ ions, resulting in a decrease in pH. This condition is detected by chemoreceptors in the brain, prompting an increase in breathing rate to expel excess CO2 and restore pH balance..
Scene 19 (32m 9s)
[Audio] The human body is made up of approximately 60% water, with the majority of this water being found in the bloodstream. Water plays a vital role in many physiological processes, including the transport of nutrients and waste products. The body's ability to regulate its internal environment is crucial for maintaining proper bodily functions. The kidneys filter waste from the blood, while the liver metabolizes toxins. The lungs also play a significant role in maintaining acid-base balance by regulating the amount of carbon dioxide in the blood. The body's acid-base balance is maintained through a complex system involving buffers such as bicarbonate, which helps maintain a stable pH level. The kidneys and lungs work together to regulate the amount of bicarbonate in the blood, ensuring that the body's internal environment remains stable. The body's ability to regulate its internal environment is essential for maintaining proper bodily functions..