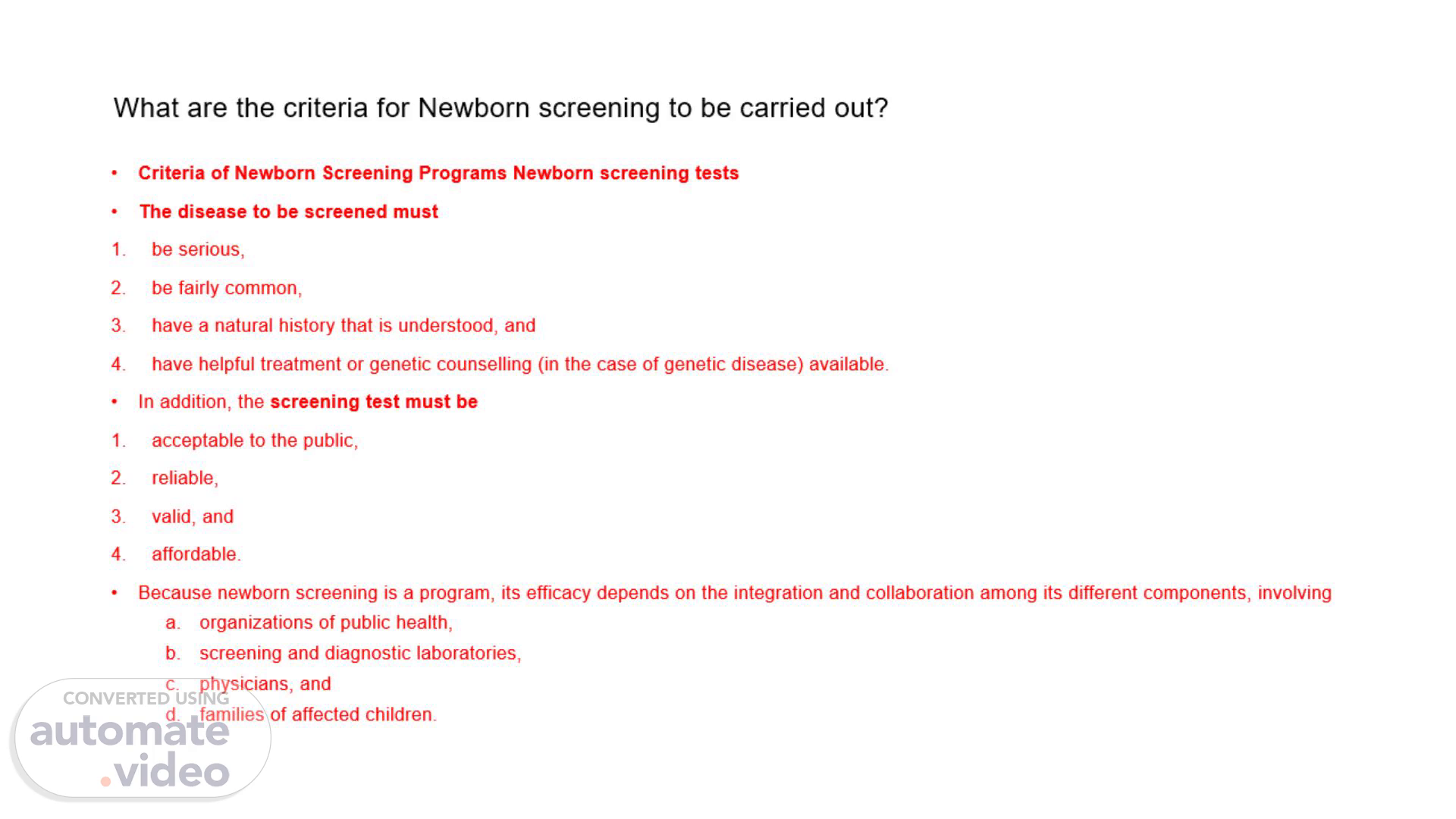
What are the criteria for Newborn screening to be carried out?
Scene 1 (0s)
[Audio] What are the criteria for Newborn screening to be carried out? Criteria of Newborn Screening Programs Newborn screening tests The disease to be screened must be serious, be fairly common, have a natural history that is understood, and have helpful treatment or genetic counselling (in the case of genetic disease) available. In addition, the screening test must be acceptable to the public, reliable, valid, and affordable. Because newborn screening is a program, its efficacy depends on the integration and collaboration among its different components, involving organizations of public health, screening and diagnostic laboratories, physicians, and families of affected children..
Scene 2 (44s)
[Audio] Describe the pathophysiology and causes of Hashimoto's disease. Hashimoto thyroiditis is characterized by the destruction of thyroid cells by various cell- and antibody-mediated immune processes. The initiating process is not well understood. The thyroid gland is typically goitrous but may be atrophic or normal in size. Antibodies binding to and blocking the thyroid-stimulating hormone (TSH) receptor have also been described and may contribute to further impairment in thyroid function. The result is inadequate thyroid hormone production and secretion, although, initially, both preformed thyroxine (T4) and triiodothyronine (T3) may "leak" into the circulation from damaged cells. Patients with Hashimoto thyroiditis have antibodies to various thyroid antigens, the most frequently detected of which include antithyroid peroxidase (anti-TPO), antithyroglobulin (anti-Tg), and, to a lesser extent, TSH receptor-blocking antibodies. Nevertheless, a small percentage of patients with Hashimoto thyroiditis (approximately 10-15%) may be antibody-negative. Other antithyroid antibodies found in AITD (including Hashimoto thyroiditis) include thyroid-stimulating antibody and cytotoxic antibody. The most common and early presenting symptoms of hypothyroidism, such as fatigue, constipation, dry skin, and weight gain, are nonspecific. Weight gain due to hypothyroidism is usually no greater than 10% of the baseline euthyroid weight and is mostly attributable to fluid accumulation in interstitial tissues. Other symptoms Cold intolerance Voice hoarseness and pressure symptoms in the neck from thyroid enlargement Slowed movement and loss of energy Decreased sweating Mild nerve deafness Peripheral neuropathy Menstrual irregularities (typically menorrhagia, infertility, and loss of libido): Increased prolactin secondary to increased thyrotropin-releasing hormone (TRH) leads to decreased luteinizing hormone (LH) and follicle-stimulating hormone (FSH) and to decreased response to gonadotropin-releasing hormone (GnRH). The result is anovulatory cycles with menstrual irregularities..
Scene 3 (3m 21s)
[Audio] List and explain 5 causes of hypothyroidism. Inflammation of the Thyroid Gland (e.g., Hashimoto's Thyroiditis): Mechanism: Inflammation leads to the destruction of thyroid cells, reducing their ability to produce hormones. Hashimoto's thyroiditis, an autoimmune condition, is a common example where the immune system mistakenly targets the thyroid gland with autoantibodies. Outcome: This results in low levels of thyroid hormones, causing symptoms like fatigue, weight gain, and cold intolerance. Failure of the Pituitary to Produce Enough TSH: Mechanism: The pituitary gland secretes thyroid-stimulating hormone (TSH), which signals the thyroid to produce hormones. Damage to the pituitary (e.g., due to a tumor, surgery, or radiation) can lead to secondary hypothyroidism, where the thyroid is under-stimulated despite being otherwise healthy. Outcome: Inadequate stimulation by TSH reduces thyroid hormone production, slowing metabolism and causing hypothyroid symptoms. Medical Treatment or Surgery Removing Part of the Thyroid: Mechanism: Treatments for hyperthyroidism, thyroid cancer, or goiter may involve radioactive iodine therapy or surgical removal of part or all of the thyroid gland. Outcome: These procedures reduce the gland's capacity to produce hormones, often leading to hypothyroidism, requiring lifelong thyroid hormone replacement therapy. Symptoms Associated with Slow Metabolism: Mechanism: Hypothyroidism, regardless of the cause, slows metabolic processes due to insufficient thyroid hormone levels. This leads to symptoms such as weight gain, dry skin, constipation, cold intolerance, and bradycardia. Outcome: Slower metabolism affects energy levels, body temperature regulation, and overall functioning. Iodine Deficiency (Additional Cause): Mechanism: Iodine is essential for the production of thyroid hormones (T3 and T4). Inadequate iodine intake leads to reduced hormone synthesis, causing hypothyroidism. Prevalence: This is common in regions with low dietary iodine, although it is rare in areas where iodized salt is widely available. Outcome: Prolonged iodine deficiency can cause hypothyroidism and goiter (enlarged thyroid)..
Scene 4 (6m 5s)
[Audio] Write up the principle behind Immunology Electrochemiluminescence (ECL) with some examples. Electrochemiluminescence (ECL) is an analytical technique combining electrochemical and luminescent methods to detect analytes with high sensitivity and specificity. It uses labeled antibodies or antigens that emit light when stimulated by an electrical current in a reaction cell. The light intensity correlates with the analyte concentration. ECL is widely used in clinical diagnostics, such as detecting hormones, cardiac markers, and infectious diseases. Examples include thyroid function tests, troponin levels for heart conditions, and viral load quantification..
Scene 5 (6m 53s)
[Audio] Discuss the acid-base disturbances in mixed disorders. Mixed acid-base disorders occur when two or more primary acid-base imbalances are present simultaneously. They are identified when pH, PaCO2, and HCO3- values do not align with expected compensatory mechanisms. Common combinations include metabolic acidosis with respiratory acidosis, metabolic acidosis with alkalosis, or respiratory acidosis with alkalosis. Tools like the delta gap, Winter's formula, and anion gap calculations help in diagnosis. Causes include renal failure, critical illness, and sepsis. Managing mixed disorders is complex, requiring careful interpretation of blood gas results and tailored treatment strategies..
Scene 6 (7m 44s)
[Audio] Describe how ISE and Photometry work. And give an example of each. Ion-Selective Electrode (ISE): ISE measures the concentration of specific ions in a sample using selective membranes that allow only the target ion to pass. The electrical potential generated by ion activity is measured and correlated to the ion concentration. An example is the measurement of sodium or potassium levels in blood. Photometry: Photometry measures the concentration of substances in a sample by assessing the absorption of light at specific wavelengths. The amount of light absorbed is proportional to the concentration of the analyte. An example is determining glucose levels in blood through colorimetric assays..