Quality Improvement Presentation Poster Barbara Polo Capella University Evidence-Based Practice for Patient-Centered Care and Population Health Evidence-Based Practice Implementation Plan June 26, 2023
Scene 1 (0s)
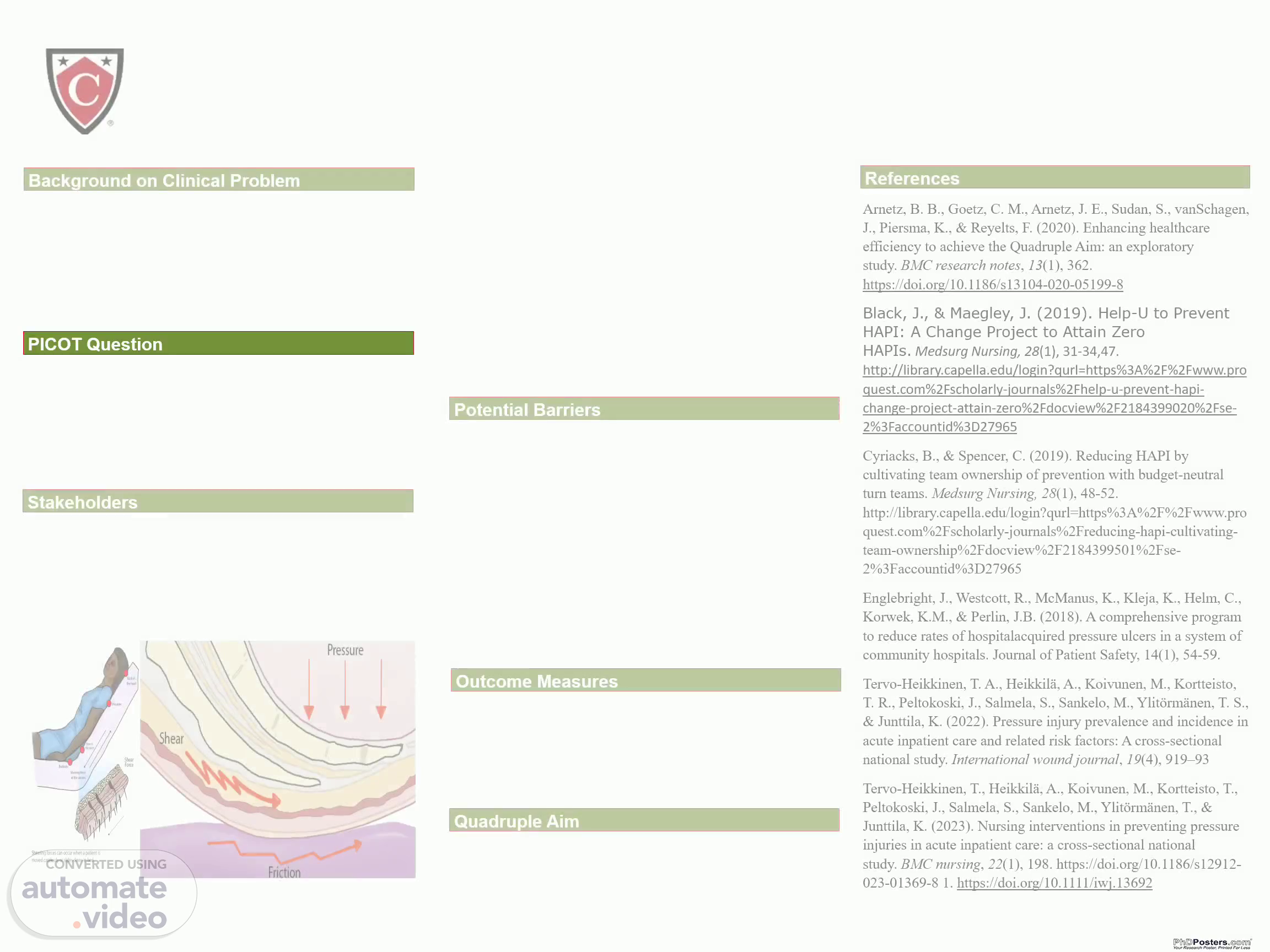
[Audio] Hospital-acquired pressure injuries on two medical-surgical units were identified as financial and patient outcome concerns (Black, 2019). There is currently a process in place for repositioning the patient every two hours, but it is not always performed. PICOT questions are the following; In adult inpatients (P), does the implementation of a comprehensive pressure injury prevention program by nurses (I), compared to standard pressure injury prevention practices (C), result in a reduction in the occurrence of pressure injuries (O) during the hospital stay (T)? Stakeholders include inpatient nurse, patient care tech, physicians, wound care nurse, charge nurse/ floor managers. Action plans would include skin inspection within 8 hours upon admission, every time there is a change in condition, and prior to discharge from the hospital, the Braden risk scoring tool would be utilized for every shift change, daily auditing documentation of patient repositioning, yearly hospital acquired pressure injury education for nurses and CNAs, assessing malnutrition within a week of admission. The suggested action plans are logical and achievable because they are consistent with recognized best practices for enhancing patient safety, reducing problems, and delivering adequate treatment. They promote early detection, prompt action, education, and preventative measures to enhance patient outcomes and treatment quality. Potential Barriers include resistance to change. To mitigate this, engage stakeholders early in the process and address concerns. The second is a lack of clear expectations. To mitigate this, the administration should set clear goals and objectives. The third is a lack of resources. To mitigate this, assess resources and identify any gaps and limitations. The fourth is a lack of communication. To solve this, provide regular updates. Lastly, is the misunderstanding of the evidence related to pressure injuries. The organization can provide continuing education and training to resolve this. Outcome Measures: Current pressure injury data is 5 hospital acquired pressure injury cases per 1,000 patient days, cases down to three cases in one month, pressure injury cases are down to two in 3 months and hospital acquired pressure injury cases down to 1 case in 6 months. The outcome measurements motivate team members to offer high-quality treatment and a great patient experience. While a productivity emphasis needs outputs and puts pressure on stakeholders to produce results, an efficiency focus deals with modification of processes and necessitates organizational transformation. Thus, ideally, a focus on efficiency should enable staff to accomplish performance metrics while boosting workplace well-being since resources and procedures are more efficient, and team members are working at the top of their abilities. For the Quadruple Aim, patient experience improved, population health improved, healthcare costs were reduced, and health care provider work lives were evaluated and improved. Hospital-acquired pressure injuries affect 1 in 30 patients and cause 60,000 fatalities annually (Englebright et al., 2018). In conclusion, pressure redistribution, team collaboration, and improved education should be routinely used to control hospital acquired pressure injury risk in acute hospitals. Implementing evidence-based practices and involving stakeholders promotes teamwork and communication. One way to avoid Hospital-acquired pressure injuries is to improve movement, nutrition and address conditions that cause immobility and pressure. Collecting data allows for the application of performance metrics, such as incidence rate per 1,000 patient days, to monitor progress and suggest areas for improvement..