MECHANISM OF URINE FORMATION
Scene 1 (0s)
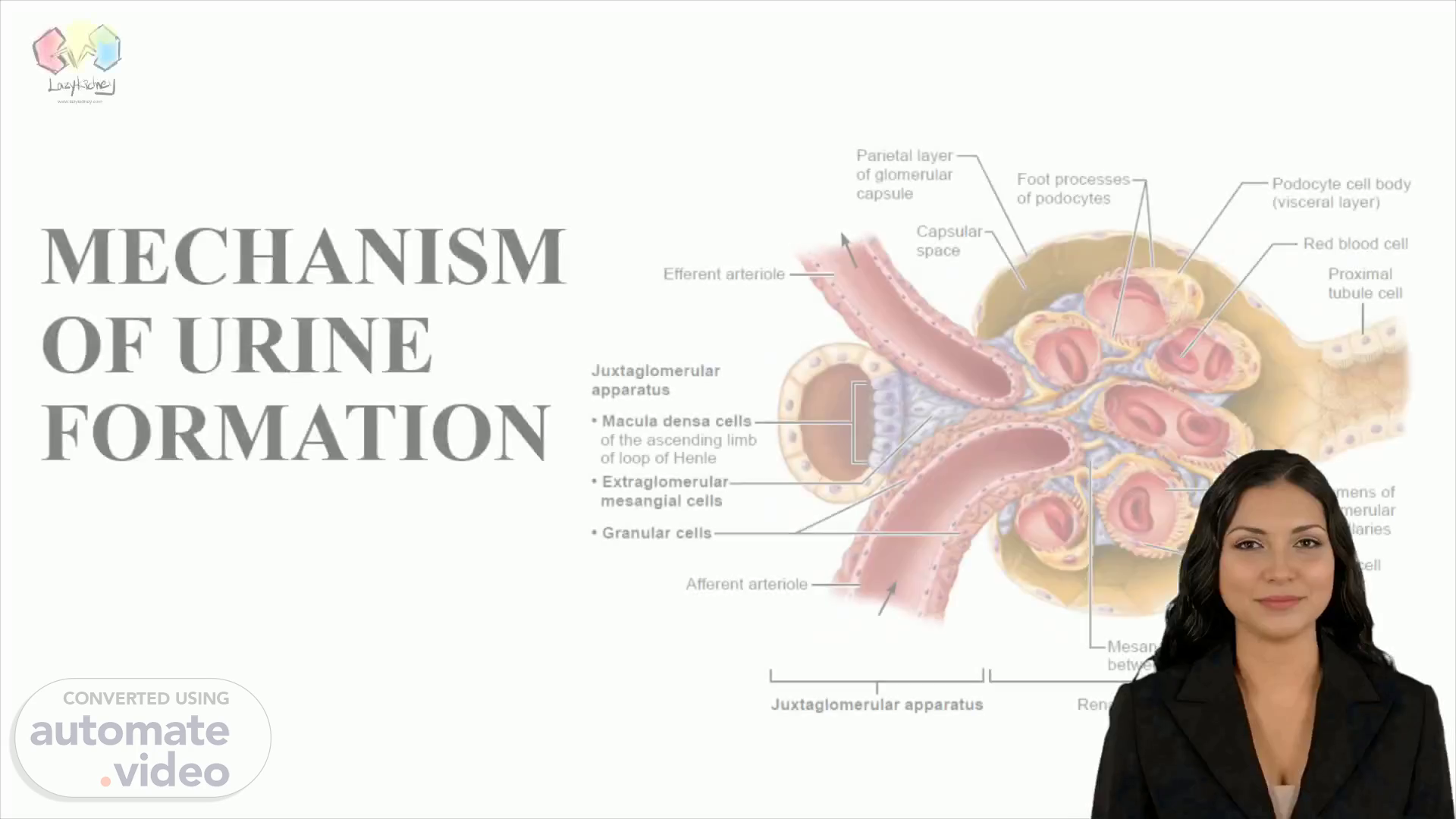
[Virtual Presenter] Today, I'm going to discuss the formation of urine in the body. The process begins with the glomerular capsule, which features an outer layer called the parietal layer. From there, the filtrate enters the space between the two layers, named the capsular space, and then passes through the efferent arteriole. At the junction of this arteriole and the capsule sits the juxtaglomerular apparatus, including the macula densa cells of the ascending loop of Henle, and the extraglomerular mesangial cells. Granular cells, foot processes of podocytes, and mesangial cells between capillaries are all a part of the renal corpuscle. Subsequently, the filtrate passes through the podocyte cell body, the red blood cells, and into the proximal tubule cell. Finally, it reaches the lumens of the glomerular capillaries, undergoing filtration by the endothelial cells. This is the mechanism of how urine is formed in the body..
Scene 2 (1m 5s)
[Audio] Urine formation is a complex process that involves many components. Glomerular filtration, tubular reabsorption, and tubular secretion are the main steps that need to take place for successful urine formation. Glomerular filtration is regulated by both intrinsic and extrinsic control, and the net filtration pressure can be calculated accordingly. All of these steps lead to the production and transport of both dilute and concentrated urine. Several structures, including glomerular structures, macula densa cells, proximal tubule cells, as well as endothelial cells of glomerular capillaries, are essential for this process..
Scene 3 (1m 50s)
[Audio] Urine formation is an important process for maintaining our body's fluid and electrolyte balance. It involves three key steps: Glomerular Filtration, Tubular Reabsorption and Tubular Secretion. Glomerular Filtration separates waste products, like urea, from the blood and sends them to the renal tubules. Then, the renal tubules take up essential nutrients, such as glucose and amino acids, and excrete excess electrolytes or hormones, such as sodium, chloride, renin and angiotensin. The collecting ducts further concentrate or dilute urine depending on the body's needs..
Scene 4 (2m 35s)
[Audio] Urine formation is an intricate process, managed by an assortment of cells and structures. The glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, podocyte foot processes, mesangial cells between capillaries, proximal tubule cells, glomerular capillary endothelial cells and red blood cells are the main parts of this process. The imperative role of this system is in regulating the filtration of the blood, the reclamation of essential nutrients and water, whilst safeguarding the body from expelling needed elements. This leaves us with urine, a complex combination of waste products that must be expelled from the body..
Scene 5 (3m 23s)
[Audio] Urine formation is a complex process that involves many different organs and components. The glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, and endothelial cells of glomerular capillaries, and red blood cells, all play a significant role. Additionally, tubular secretion is essential in aiding the body's chemical balance by selectively adding or removing substances to and from the renal tubules and the collecting ducts..
Scene 6 (4m 5s)
[Audio] Our slide today discussed the formation of urine, a complex process regulated by blood vessels, cells, and renal tubules. Every minute, 1200ml of blood is filtered and processed, 120-125ml of the plasma of which is pushed into the renal tubules. Every day, 180 litres of blood-derived fluid is processed by the kidneys, of which only 1.5 litres remains as urine while the rest is recycled back into the body. This slide presented the intricate workings of the urinary system..
Scene 7 (4m 43s)
MECHANISM OF URINE FORMATION. Mechanism of Urine Formation.
Scene 8 (4m 49s)
[Audio] In urine formation, several elements are involved, including the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. Glomerular filtration is a passive process, allowing filtration of molecules up to 3 nanometers in diameter from the blood into the glomerular capsule, while molecules larger than 5 nanometers are generally blocked. Knowing how urine formation is regulated has important implications for our health..
Scene 9 (5m 35s)
[Audio] Urine formation is a complex and regulated process that involves several components. The glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, and foot processes of podocytes, as well as mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells are all key players. The pressure of the glomerular blood, or HPg, is the principal driving force behind the water and solutes that are pushed out of the blood and across the filtration membrane. The oncotic pressure of the glomerular blood, or OPg, and the hydrostatic pressure of the capsule, or HPc, act as opposing forces, moderating the fluid lost from the glomerular capillaries. When the net filtration pressure is calculated, that is, when HPg is subtracted from OPg and HPc, the result is the amount of water and solutes that are filtered from the glomerular capillaries into the glomerular capsule. In simpler terms, the amount of fluid that filters into the glomerular capsule is decided by the pressure differential between the capsule and the blood..
Scene 10 (6m 54s)
[Audio] Net Filtration Pressure is the difference between Glomerular Filtration Pressure and Starling Resistant Pressure. Filtration of urine from the capillaries of the glomerulus into Bowman's capsule is an active process, which depends on hydrostatic pressure of glomerular capillaries and osmotic pressure of colloidal substances in the plasma. This process is regulated by different components such as glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells..
Scene 11 (7m 40s)
[Audio] Glomerular filtration is a process that filters small molecules and waste products from the body, leaving bigger molecules such as proteins and red blood cells in the bloodstream. The rate at which this occurs is called the glomerular filtration rate (GFR). Various components in the body play a role in controlling the GFR, such as the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. The net filtration pressure, the difference between the hydrostatic pressure and oncotic pressure, determines the amount of filtration that will occur - the greater the pressure, the more likely it is for filtration to occur..
Scene 12 (8m 38s)
[Audio] The glomerular filtration rate (GFR) is one of the body’s primary mechanisms for filtering out waste products from our blood. It is calculated as the volume of fluid that is filtered each minute by the kidneys. The components that make up the GFR include the total surface area for filtration, the permeability of the filtration membrane, and the net filtration pressure. These components enable our bodies to effectively remove waste and maintain healthy levels of essential substances like electrolytes, amino acids, glucose, and small proteins..
Scene 13 (9m 16s)
[Audio] The urinary system plays an important role in regulating the composition of the blood. This slide has discussed how urine formation is regulated through different pathways. In adults, the normal Glomerular Filtration Rate in both kidneys is 120-125 milliliters per minute per 1.73 square meters. It is interesting to note that the GFR is directly proportional to the Net Filtration Pressure, meaning any change in any of the pressures acting at the filtration membrane will affect both the Net Filtration Pressure and the Glomerular Filtration Rate..
Scene 14 (9m 54s)
[Audio] Glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells all act to control glomerular filtration in the kidney. Glomerular filtration rate, or GFR, is regulated by both intrinsic and extrinsic controls. Intrinsic or renal autoregulatory controls mainly act within the kidney to control GFR, while extrinsic controls from the nervous and endocrine systems help to maintain blood pressure. These two types of regulation work together to help the kidneys function optimally..
Scene 15 (10m 45s)
[Audio] In this slide we will discuss how urine formation is regulated. The components involved in this process include the glomerular capsule, juxtaglomerular apparatus, macular densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. The kidney is able to regulate urine formation through something called intrinsic controls, or renal autoregulation. This means the kidney is able to maintain a nearly constant GFR despite fluctuations in systemic arterial blood pressure. This regulatory process has two components, a myogenic mechanism, and a tubuloglomerular feedback mechanism. We hope this information has provided some insight into how the kidney regulates urine formation..
Scene 16 (11m 46s)
[Audio] Urine formation is a complex process involving a range of structures and cells. Myogenic mechanism plays an important role in its regulation as it mirrors the tendency of the vascular smooth muscle to contract when stretched, helping to keep glomerular blood pressure at a safe level. When systemic blood pressure increases, afferent arterioles constrict, limiting the amount of blood that can flow into the glomerulus and preventing an excessive increase in glomerular blood pressure. All these components work together to ensure that the production of urine remains properly regulated..
Scene 17 (12m 24s)
[Audio] The myogenic mechanism affects glomerular hydrostatic pressure in order to regulate urine formation. It involves the walls of the afferent and efferent arterioles, as well as the endothelial cells of the glomerular capillaries. When systemic blood pressure drops, the walls of the afferent arterioles dilate, resulting in an increase in glomerular hydrostatic pressure. This helps sustain a normal glomerular filtration rate and is an important element of urine formation, which is regulated in conjunction with other factors discussed in this presentation..
Scene 18 (13m 2s)
MECHANISM OF URINE FORMATION. T ubuloglomerular Feedback M echanism I s directed by the macula densa cells of the juxtaglomerular apparatus. These cells, located in the walls of the ascending limb of Henle’s loop, respond to filtrate NaCl concentration . When GFR increases, there is insufficient time for reabsorption and the concentration of NaCl in the filtrate remains high. This causes the macula densa cells to release a vasoconstrictor chemical ATP that causes intense constriction of the afferent arteriole..
Scene 19 (13m 24s)
[Audio] In this slide, we will discuss the role of the tubuloglomerular feedback (TGF) mechanism in urine formation. This feedback is generated between the macula densa cells and the afferent arterioles of the glomerulus and it helps regulate the filtration rate in order to keep the body in a state of homeostasis. If the macula densa cells detect a decrease in the sodium chloride concentration of the filtrate, they release ATP, causing vasodilation of the afferent arterioles, thereby increasing the net filtration pressure and glomerular filtration rate, hence, allowing the kidney to filter more urine. However, if the macula densa cells detect too fast of a flow rate, they cease ATP release and this leads to the constriction of the afferent arterioles, resulting in decreased filtration..
Scene 20 (14m 17s)
[Audio] Urine formation is a highly regulated process to ensure that the correct amount of fluid, electrolytes, and waste products are excreted. This process begins with the glomerular capsule which filters the blood to create a filtrate that then passes through the juxtaglomerular apparatus. Subsequently, the filtrate is modified by macula densa cells, extraglomerular mesangial cells, granular cells, and podocyte foot processes. Various cells such as mesangial cells between glomerular capillaries, proximal tubule cells, glomerular capillary endothelial cells, and red blood cells have vital roles in the regulation of urine formation. Intrinsic controls are accountable for maintaining a relatively constant glomerular filtration rate within the range of eighty to 180 millimeters of mercury in arterial pressure. Nevertheless, this autoregulatory mechanism ceases to function if the mean arterial pressure drops below eighty millimeters of mercury..
Scene 21 (15m 23s)
[Audio] Regulation of urine formation in our bodies is an incredible process, controlled by various factors. These include the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between the capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. Furthermore, two external controls are responsible for regulating the glomerular filtration rate - neural and hormonal mechanisms. This allows for maintenance of systemic blood pressure, as well as protecting our kidneys..
Scene 22 (16m 9s)
[Audio] Urinary formation is controlled by a complex network of related cells and tissues. These include the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, podocyte foot processes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. The sympathetic nervous system also plays an important part in regulating the renal processes, ensuring they meet the body's requirements. In normal circumstances, when the sympathetic nervous system is inactive, the renal blood vessels are widened and renal autoregulation occurs..
Scene 23 (16m 56s)
[Audio] Urine is produced by the body through a precise process, involving several components. The glomerular capsule and the juxtaglomerular apparatus filter the incoming blood, while the macula densa cells, extraglomerular mesangial cells, granular cells and the foot processes of podocytes reabsorb certain substances. Additionally, mesangial cells sit between the capillaries, proximal tubule cells and the endothelial cells of the glomerular capillaries, which absorb and secrete necessary compounds. Red blood cells also play an important role. Generally, urine formation is regulated by the sympathetic nervous system, though during stressful or emergency situations, neural activity may take precedence and override the kidneys' autoregulatory mechanisms..
Scene 24 (17m 50s)
[Audio] Urine formation is a complex process involving numerous organs and structures. Glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, the foot processes of the podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of the glomerular capillaries, and red blood cells all take part in this process. Knowing how these organs and structures contribute to urine production is essential to comprehending how the sympathetic nervous system regulates it. Norepinephrine is secreted from sympathetic nerve fibers and epinephrine from the adrenal medulla to act on alpha-adrenergic receptors on the vascular smooth muscle, causing it to constrict the afferent arterioles, thus reducing the amount of filtrate created..
Scene 25 (18m 44s)
[Audio] Urine formation is regulated through the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. The sympathetic nervous system stimulates the macula densa cells, leading to the renin angiotensin mechanism. Additionally, it directly triggers the granular cells to release renin..
Scene 26 (19m 21s)
[Audio] Renin is released by granular cells and, when it acts on angiotensinogen, a molecule produced in the liver, it produces angiotensin I, which is then converted to angiotensin II. Angiotensin II is the final product of the renin-angiotensin mechanism, and is created by angiotensin converting enzyme which is associated with capillary endothelium in various body tissues, mainly in the lungs. The renin-angiotensin mechanism has a significant role in urine formation and regulation, and is a complicated process..
Scene 27 (19m 58s)
[Audio] Urine formation is a complex process that involves multiple structures and processes. The glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells all act in unison to produce and secrete urine. Also playing an equally important role is the renin-angiotensin mechanism, which is responsible for stabilizing systemic blood pressure and extracellular fluid volume. This mechanism is mainly driven by angiotensin II, a powerful vasoconstrictor that stimulates reabsorption of sodium..
Scene 28 (20m 49s)
[Audio] Urine formation is a complex process heavily regulated by the biological workings of the body. We'll be looking at the major components that make it up, including the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. This combination ultimately leads to the Renin-angiotensin mechanism, which assists in controlling the volume of circulating blood and regulating the body's water balance. Notably, Angiotensin II promotes the hypothalamus to launch antidiuretic hormone and triggers the hypothalamic thirst center, both helping to raise the volume of circulating blood. Healthcare professionals should have a thorough knowledge of these complex components and their interactions to effectively understand the regulation of the water balance in the body..
Scene 29 (21m 55s)
[Audio] A complex network of cells and vessels regulate the formation of urine. Glomerular capsules, juxtaglomerular apparatuses, macula densa cells, extraglomerular mesangial cells, granular cells, and foot processes of podocytes are all part of the process that filters blood and produces a filtrate that can be modified into urine. Furthermore, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells all contribute to the reabsorption of fluid and the control of the ultimate urine composition. The renin-angiotensin mechanism also plays a role in changes in the peritubular capillary hydrostatic pressure, thus affecting the fluid reabsorbed. Ultimately, the formation of urine is designed to achieve the optimal composition for the body..
Scene 30 (22m 52s)
[Audio] Observing the different elements which participate in the regulation of urine formation, the renin-angiotensin mechanism stands out as an important component. Angiotensin II is responsible for regulating the glomerular filtration rate by contracting the glomerular mesangial cells, thus decreasing the total surface area of glomerular capillaries available for filtration..
Scene 31 (23m 17s)
[Audio] Urine formation is regulated by numerous components, including the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, the foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, the endothelial cells of the glomerular capillaries, and red blood cells. Reduced stretch of the granular cells is one of the factors that can independently or collectively cause the release of renin when mean systemic blood pressure is below 80 mmHg..
Scene 32 (23m 54s)
[Audio] Urine formation involves a complex process with the body's regulation system and several organs, including the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. A hormone called renin is released when several factors, including stimulation of the granular cells from the activated macula densa cells, triggers it. When the macula densa cells detect a low concentration of sodium chloride in the filtrate, they activate the granular cells to release renin. This can be due to a decrease in ATP or an increased prostaglandin PGE2 release, or both..
Scene 33 (24m 50s)
[Audio] Urine formation is a complex process, regulated by several structures in the glomerulus, glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells and granular cells. The foot processes of podocytes, mesangial cells between the capillaries, and endothelial cells of the glomerular capillaries, and red blood cells, all contribute. Additionally, several factors, individually or in unison, can trigger the release of renin, which includes direct stimulation of granular cells through β1-adrenergic receptors by renal sympathetic nerves..
Scene 34 (25m 32s)
[Audio] The glomerulus is the core element in urine formation, functioning for the kidney to effectively filter out toxins and unwanted substances from the body. The glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells are all involved in regulating the glomerular filtration. The renal cells also generate a variety of chemicals which act as paracrines, for example prostaglandin E2, intrarenal angiotensin II, and adenosine, that can influence the glomerular filtration rate..
Scene 35 (26m 22s)
[Audio] We will be discussing the process of tubular reabsorption in the kidney which begins when the filtrate enters the proximal tubules. This process is essential to maintain our plasma volume and is selective and regulated by various structures such as the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries and red blood cells. Understanding this process helps us understand how our bodies maintain homeostasis..
Scene 36 (27m 4s)
[Audio] Urine formation in the nephron is regulated by several components, including the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, and endothelial cells of the glomerular capillaries. After passing through the glomerular capsule, the filtrate is then reabsorbed by the proximal tubule. Reabsorbed substances can follow either the transcellular route, which involves the luminal membrane, the cytosol, and the basolateral membrane of the tubule cell, before the endothelium of the peritubular capillaries, or the paracellular route, which follows intercellular spaces between cells, to reach the blood..
Scene 37 (27m 56s)
[Audio] In this slide we will discuss how substances move in the proximal nephron. The proximal nephron includes a variety of cells and structures, such as the glomerular capsules, Juxtapolomerular apparatus, macula densa, and extraglomerular mesangial cells. These cells and structures help regulate urine formation. Moving on to movement of substances, movement in the paracellular route between tubule cells is limited, as the cells are connected by tight junctions. In the proximal nephron, however, these tight junctions are 'leaky', and allow some important ions such as calcium, magnesium, potassium, and sodium, through the paracellular route..
Scene 38 (28m 44s)
[Audio] The slide illustrates how solutes and water move from the glomerulus to the bladder via the nephron. Filtrate is pushed through the lumen of the tubule cells by pressure. The walls of the tubule cells have a luminal membrane, a basolateral membrane, and tight junctions between them, collectively forming the paracellular route. In addition to the paracellular route, transcellular routes involve transport across the luminal membrane, diffusion through the cytosol, transport across the basolateral membrane, and movement through the interstitial fluid and into the capillary. Urine is formed via active and passive transport..
Scene 39 (29m 26s)
[Audio] The formation of urine in healthy kidneys is an intricate and regulated process, encompassing multiple components. These include the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. When the kidneys are healthy, organic nutrients like glucose and amino acids are completely reabsorbed by the body in order to maintain or restore normal plasma concentrations. Furthermore, water and many ions are regulated and adjusted in response to hormones. All of these components are essential for both the formation of urine and absorption of key nutrients by the body..
Scene 40 (30m 23s)
[Audio] Sodium is crucially involved in urine formation, and is almost always actively reabsorbed. It is the most predominant cation in the filtrate. Therefore it is essential for us to gain insight into the different processes and cells associated with sodium reabsorption. This process occurs through the transcellular route, comprising several components of the urinary system. Included are the glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, podocyte foot processes, mesangial cells located between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells..
Scene 41 (31m 12s)
[Audio] Urine formation is a complex process that involves several parts of the nephron. It requires components such as glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells. A vital part of this mechanism is the active reabsorption of sodium (Na+) from the tubule cell by a Na-K ATPase pump present in the basolateral membrane and then it is pushed by the water flow into the peritubular capillaries. Knowing how these processes collaborate will provide us additional understanding regarding how urine is formed..
Scene 42 (32m 4s)
[Audio] The glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between the capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells all have important roles in urine formation. In each tubule segment, two main processes occur which bring about active Na+ reabsorption. Firstly, active pumping from the tubule cells causes an electrochemical gradient that creates passive entry of Na+ at the luminal face. This entry is accomplished through secondary active transporters, symport or antiport, or through facilitated diffusion through channels..
Scene 43 (32m 55s)
MECHANISM OF URINE FORMATION. Mechanism of Urine Formation.
Scene 44 (33m 1s)
[Audio] Sodium reabsorption is essential for urine formation regulation. It is achieved through primary active transport, which utilizes energy and permits reabsorption of virtually anything, including water. Secondary active transport is used to take up substances like glucose, amino acids, lactate and vitamins. In the proximal tubule, reabsorption of nutrients, water and ions occurs. This combination of reabsorption leads to a balance in urine formation, allowing us to maintain a healthy condition..
Scene 45 (33m 40s)
[Audio] Having studied the anatomy and physiology of the nephron, let's discuss how its components regulate the transport of substances from the glomerular filtrate to the urine. Through active reabsorption, the majority of the filtered ions and water are recycled back to the bloodstream, leaving only a minimal amount of the glomerular filtrate to be excreted as urine. A key point to consider here is the transport maximum, or Tm. This value indicates the maximum rate at which a particular substance can be reabsorbed. It is determined by the quantity of transporters in the nephron membrane. A greater number of transporters leads to a higher Tm value for a given substance. This explains why substances such as glucose, which the body needs to retain, have high Tm values, and substances that are not useful have lower Tm values..
Scene 46 (34m 38s)
[Audio] Passive tubular reabsorption plays a role in urine formation by comprising osmosis, diffusion, and facilitated diffusion. Through this process, substances move down their electrochemical gradients, only allowing for the excess substances that the transporters are bound to be excreted in the urine. This is an important mechanism as it ensures that the right balance of substances is maintained..
Scene 47 (35m 6s)
[Audio] The glomerular capsule captures substances from the plasma, including many proteins, and delivers them to the filtrate by ultrafiltration. Water and solutes pass through the pores of the endothelial cells within the glomerular capillaries and arrive at the juxtaglomerular apparatus, a specialised region of the afferent and efferent arterioles and the macula densa cells of the distal convoluted tubule. The macula densa cells sense the filtrate osmolality, triggering paracrine signals that result in the release of renin. Renin catalyses the production of angiotensin II, which stimulates aldosterone secretion from the adrenal cortex. Aldosterone binds to mineralocorticoid receptors in the collecting ducts and increases the permeability of these cells to Na+ in the form of corticomedullary osmotic gradients. The movement of Na+ and other solutes establishes a strong osmotic gradient, and water moves by osmosis into the peritubular capillaries. This is a process aided by transmembrane proteins called aquaporins that form water channels across cell membranes. In continuously water-permeable regions of the renal tubules, such as the PCT, aquaporins are constant components of the tubule cell membranes. Urine formation is thus regulated through a complex system of processes that involve the components listed above..
Scene 48 (36m 37s)
[Audio] A greater understanding has been developed to see how treating everyone with respect and fairness can result in a better society for all. Aquaporins channels are always present, which makes it unavoidable for the body to absorb water in the proximal nephron, no matter if the body is over- or underhydrated. This water flow is known as obligatory water reabsorption..
Scene 49 (37m 2s)
[Audio] Regulation of urine formation is a complex process involving a number of components of the nephron. The glomerular capsule, juxtaglomerular apparatus, macula densa cells, extraglomerular mesangial cells, granular cells, foot processes of podocytes, mesangial cells between capillaries, proximal tubule cells, endothelial cells of glomerular capillaries, and red blood cells all contribute to the process. This combination of parts allows for filtering and concentration of substances, as well as managing the passive reabsorption of solutes and lipid-soluble compounds. As a result, the rate of filtration and the composition of the filtrate can be controlled; this in turn leads to the formation of urine..
Scene 50 (37m 54s)
[Audio] The formation of urine in humans is regulated by several structures and entities. The glomerular capsule, the juxtaglomerular apparatus, the macula densa cells, the extraglomerular mesangial cells, the granular cells, the foot processes of podocytes, the mesangial cells between capillaries, the proximal tubule cells, the endothelial cells of glomerular capillaries and the red blood cells all play their part. Any plasma proteins that squeeze through the filtration membrane are removed from the filtrate in the proximal tubule by endocytosis and digested to their amino acids, which are then moved into the peritubular blood. In conclusion, this is how urine is formed..