Immunity and Inflammation powerpointwithoutvoiceover (2)
Scene 1 (0s)
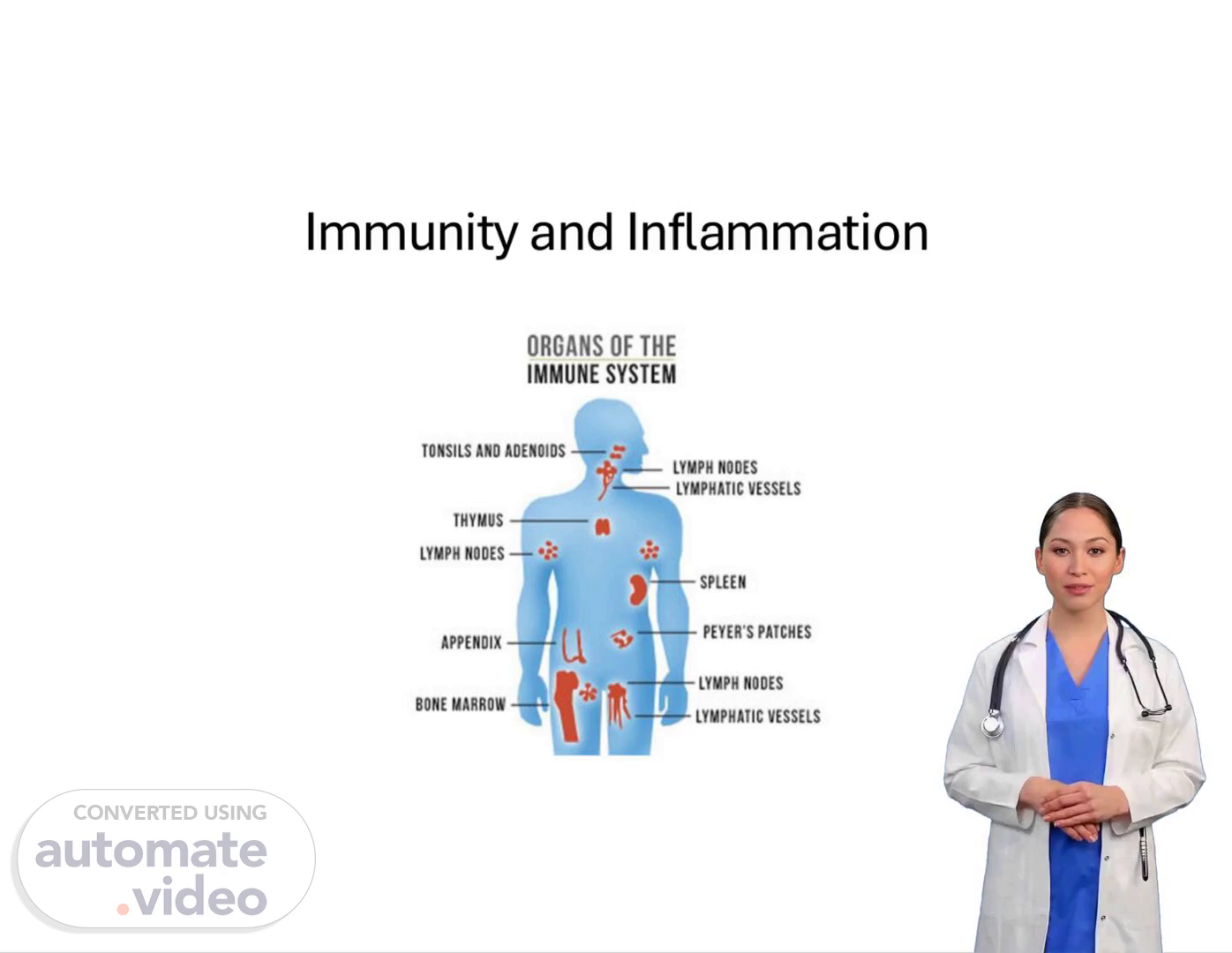
[Virtual Presenter] Immunity refers to the body's ability to defend itself against pathogens such as bacteria, viruses, fungi, and parasites. The immune system consists of various cells, tissues, and organs that work together to protect the body from infection and disease. The main components of the immune system include the lymph nodes, spleen, thymus, bone marrow, and white blood cells. These components are responsible for recognizing and eliminating pathogens, as well as producing antibodies to neutralize toxins and fight off infections. The immune system also plays a crucial role in the development of autoimmune disorders, where the body mistakenly attacks its own tissues. Inflammation is a complex process that involves the activation of immune cells, the release of chemical signals, and the recruitment of immune cells to the site of injury or infection. Inflammation can be acute or chronic, depending on the severity and duration of the insult. Acute inflammation is typically characterized by redness, swelling, heat, pain, and loss of function, while chronic inflammation is often associated with tissue damage and scarring. Inflammation can have both beneficial and detrimental effects on the body, depending on the context and duration. For example, acute inflammation can help to clear infections, but chronic inflammation can lead to conditions such as arthritis, diabetes, and cardiovascular disease. The relationship between immunity and inflammation is closely linked. Immune responses can trigger inflammation, which can then exacerbate the underlying condition. Conversely, inflammation can also stimulate immune responses, leading to further inflammation and tissue damage. Understanding the interplay between immunity and inflammation is essential for developing effective treatments for various diseases. By studying the mechanisms of immunity and inflammation, researchers can identify potential therapeutic targets and develop new treatments that target specific pathways involved in these processes..
Scene 2 (2m 14s)
[Audio] The pathophysiology of immunity and inflammation involves complex interactions between various cellular and molecular components. The immune system is designed to protect against infection and disease, but it can also cause damage if not properly regulated. When an individual is exposed to a pathogen, the immune system responds by activating its various defense mechanisms. However, if the immune response becomes overactive or uncontrolled, it can lead to tissue damage and chronic inflammation. Inflammation is a natural response to injury or infection, but excessive or prolonged inflammation can have negative consequences. Chronic inflammation has been linked to various diseases such as arthritis, diabetes, and cardiovascular disease. The underlying causes of chronic inflammation are multifactorial and involve genetic predisposition, environmental factors, and lifestyle choices. The nursing process is essential in managing clients with alterations in immunity and inflammation. The nursing process includes assessment, diagnosis, planning, implementation, and evaluation. Nurses must assess the client's condition, diagnose any underlying conditions, develop a plan of care, implement the plan, and evaluate the effectiveness of the care provided. Clinical judgment plays a crucial role in this process, allowing nurses to make informed decisions about the client's care. Nurses play a vital role in promoting healthy habits and preventing disease. They can educate clients on the importance of maintaining a healthy diet, exercising regularly, and avoiding harmful substances. Nurses can also provide emotional support and counseling to clients who are experiencing stress or anxiety related to their illness. By understanding the pathophysiology of immunity and inflammation, nurses can provide more effective care to clients experiencing these alterations. This knowledge enables nurses to identify potential complications and take proactive measures to prevent them. Nurses can also work collaboratively with other healthcare professionals to ensure comprehensive care for clients with alterations in immunity and inflammation..
Scene 3 (4m 34s)
[Audio] The immune system is a complex network of cells, tissues, and organs that work together to protect our bodies from harmful invaders such as bacteria, viruses, and parasites. It is not just confined to one specific area of the body, but is spread throughout. This means that the immune system is actively involved in many different areas of our body to keep us healthy. The bone marrow is a spongy tissue found in our bones, where immune cells are produced and multiplied. It is an essential part of our immune system, as it continuously creates new immune cells to help fight off infections and diseases. The thymus is located behind the breastbone and in front of the trachea. This organ helps to mature and produce T-cells, which are crucial in the immune response. The spleen is about the size of a fist, and located in the abdomen. It filters the blood and helps to remove old or damaged red blood cells. Tonsils are two oval-shaped masses located in the back of the throat. They are a part of the body's first line of defense and help to trap and remove harmful germs that enter through the mouth and nose. Lymph nodes are small, bean-shaped structures located throughout the body. They serve as meeting points for different immune cells, and a swollen lymph node is often a sign of an active immune response. Mucous membranes line various parts of our body, such as our gastrointestinal tract and lungs. They help to trap and expel harmful substances before they can enter our body. The skin forms a physical barrier, preventing harmful germs from entering our body and causing infection. The gut is where a significant portion of our immune system is located. It is estimated that about 80% of our immune system is located in the gut. The gut contains a diverse community of microorganisms, known as the microbiome, which plays a vital role in regulating our immune response..
Scene 4 (6m 37s)
[Audio] The human body is made up of trillions of cells, each with its own unique characteristics and functions. These cells work together to form organs, which in turn make up the entire body. The human body is also composed of various systems, including the nervous system, circulatory system, respiratory system, digestive system, endocrine system, immune system, musculoskeletal system, and others. Each system has its own specific functions and plays a vital role in maintaining the overall health and well-being of the individual. The immune system is one of the most critical components of the human body, responsible for protecting the body against external threats such as bacteria, viruses, and other pathogens. The immune system consists of two main parts: the innate immune system and the adaptive immune system. The innate immune system provides immediate protection against infections, while the adaptive immune system takes longer to develop but provides long-term immunity. Both systems work together to provide comprehensive protection against diseases. The immune system also plays a key role in eliminating toxins and waste products from the body. The immune system is regulated by a complex system of hormones and neurotransmitters that help maintain homeostasis and prevent disease. The immune system is also influenced by lifestyle factors such as diet, exercise, and stress levels. These factors can either support or hinder the functioning of the immune system. The immune system is a highly dynamic and responsive system that is capable of adapting to changing conditions. It is also capable of remembering past infections and mounting a more effective response to future infections. This ability to remember and adapt is what makes the immune system so powerful and effective. The immune system is also closely linked to the nervous system, and both systems work together to maintain overall health and well-being. The immune system is a critical component of the human body, and its proper functioning is essential for maintaining good health and preventing disease..
Scene 5 (8m 59s)
[Audio] The percentage of neutrophils in a healthy individual's blood is typically around 55-70%. These cells play a crucial role in responding to injury and fighting off invading pathogens such as bacteria and viruses. Through phagocytosis, neutrophils engulf and digest bacteria, helping to prevent infection. Immature neutrophils, often referred to as "bands" or "stabs," indicate ongoing infection or inflammation. The percentage of lymphocytes in a healthy individual's blood should be between 20-40%. Lymphocytes are specialized cells that fight chronic bacterial infections and acute viral infections. There are two main types of lymphocytes: T cells and B cells. Monocytes are responsible for cleaning up damaged tissues and producing interferon, which enhances the immune response. Monocytes also perform phagocytosis, helping to eliminate pathogens. Eosinophils are involved in allergic reactions and parasitic infections, and their numbers decrease as the allergic reaction subsides. Eosinophils also engage in phagocytosis and help to reduce inflammation and infection. Basophils release histamine, serotonin, and heparin, and are also known as mast cells. Basophils perform phagocytosis and contribute to reducing inflammation and infection..
Scene 6 (10m 34s)
[Audio] The immune system plays a vital role in protecting our bodies from pathogens such as bacteria, viruses, and fungi. One of its primary functions is to prevent infections by recognizing and attacking these foreign invaders. This process is known as immunity. The immune system achieves this through various mechanisms, including the production of antibodies that specifically target and neutralize pathogens. Another key aspect of immunity is the activation of immune cells, such as white blood cells, which help to eliminate infected cells and tissues. Additionally, the immune system can also trigger inflammation, a protective response to injury, disease, or irritation. However, sometimes the immune system can go awry, leading to autoimmune disorders where the body's own tissues are attacked by the immune system. Autoimmune disorders can result in a range of symptoms, from mild to severe, and can have significant impacts on a person's quality of life. Understanding the concepts of immunity, inflammation, and autoimmunity is essential for nurses and healthcare professionals to provide effective care to patients with these conditions..
Scene 7 (11m 46s)
[Audio] The immune system has two main components: innate immunity and adaptive immunity. Innate immunity provides immediate defense against infections and foreign invaders through various components such as skin, mucous membranes, normal flora, white blood cells, gastrointestinal tract, interferon, hydrochloric acid, cytokines, natural killer cells, and macrophages. Adaptive immunity is a more specific line of defense that develops after exposure to antigens. When the body encounters an antigen, it mounts a rapid and destructive response, and also retains a memory of the antigen for future encounters. This allows the body to develop a targeted response to specific pathogens. B lymphocytes and T lymphocytes are key players in adaptive immunity. B lymphocytes produce antibodies to fight off pathogens, while T lymphocytes directly attack infected cells. There are two main types of T lymphocytes: helper T cells and cytotoxic T cells. Both types of T cells are essential for effective immune function..
Scene 8 (13m 3s)
[Audio] The humoral immunity is mediated by antibodies produced by B cells. These antibodies play a crucial role in protecting the body from external pathogens. There are several types of antibodies, each with distinct characteristics and functions. One type of antibody, IgA, protects the surfaces of the body that are most susceptible to foreign substances, such as the respiratory, gastrointestinal, and genitourinary tracts. Another type of antibody, IgM, is the largest antibody and accounts for 5-10% of all antibodies. It is the first line of defense against infections and plays a key role in activating the immune system. IgA antibodies are also found in breast milk, where they help to strengthen the immune system of newborns. They also help to stimulate the immune system to combat foreign substances. IgD is present in low concentrations in conjunction with IgM, while IgE triggers the body's response to foreign matter such as pollen, spores, pet dander, and fungi. IgE levels are typically high in individuals with allergies. IgG is vital in warding off both bacterial and viral infections and is present in the lungs, skin, and mucous membranes. Interestingly, IgG antibodies can pass through the placenta during pregnancy to protect the fetus. Additionally, IgG antibodies may be present in individuals who experience allergic reactions to medications or milk. Overall, these different types of antibodies work together to provide comprehensive protection against a wide range of pathogens..
Scene 9 (14m 45s)
[Audio] The adaptive immune system is a complex network of cells and proteins that work together to protect the body from invading microorganisms. The immune system uses various mechanisms to defend against infections, including the activation of immune cells such as T-cells and B-cells. These cells play a critical role in the adaptive immune response, which involves the recognition and elimination of pathogens through specific immune responses. The adaptive immune system also relies on the production of antibodies, which are proteins that bind to specific antigens and neutralize them. Antibodies are produced by B-cells and are essential for providing long-term immunity against certain infections. The adaptive immune system is highly adaptable and can be triggered by exposure to specific pathogens or antigens, allowing it to mount a targeted defense against invading organisms..
Scene 10 (15m 46s)
[Audio] The human body has two main types of immunity: active and passive immunity. Active immunity is achieved by exposing the body to a pathogen, resulting in the production of antibodies. Passive immunity, on the other hand, is obtained through the transfer of pre-formed antibodies from one individual to another. There are three forms of passive immunity: natural, artificial, and acquired. Natural passive immunity occurs when antibodies are transferred from the mother to the child during pregnancy or breastfeeding. Artificial passive immunity is provided through the administration of immune globulins after exposure to a disease. Acquired passive immunity is obtained through the injection of antibodies into the body. All forms of immunity provide some level of protection against pathogens, but they differ in their duration and effectiveness. Active immunity offers more durable protection than passive immunity, as it allows the body to produce its own antibodies in response to a pathogen. The benefits of active immunity include its ability to provide lifelong protection against certain diseases, making it a crucial component of modern medicine. Passive immunity, however, provides immediate protection but is generally less effective and shorter-lived compared to active immunity. Both types of immunity play critical roles in preventing infections and diseases, and understanding their differences is essential for developing effective treatments and vaccines..
Scene 11 (17m 20s)
[Audio] Inflammation is a natural protective mechanism that helps protect our bodies from harm. It acts quickly to prevent damage caused by tissue injury or exposure to foreign substances. This rapid response is essential for our overall health and wellbeing. Inflammation leads to visible signs such as redness, swelling, and pain, and it plays a significant role in eliminating harmful microorganisms from our bodies. However, when inflammation becomes chronic, it can cause irreversible damage to tissues. The delicate balance between inflammation and the immune system is crucial for maintaining good health. Recognizing the importance of inflammation in our daily lives is vital for understanding its role in our overall health..
Scene 12 (18m 11s)
[Audio] Infection occurs when an organism invades tissues, triggering an immune response that leads to inflammation. However, this does not necessarily mean that an infectious agent is present. Inflammation can be caused by non-infectious factors such as trauma, burns, or other types of tissue injury. Therefore, it is crucial to distinguish between inflammation caused by infection and inflammation resulting from other factors. Inflammation does not always indicate the presence of an infectious agent..
Scene 13 (18m 51s)
[Audio] The five cardinal manifestations of inflammation are commonly recognized as warmth, redness, edema, pain, and decreased function. These signs occur in a specific order, with warmth typically appearing first, followed by redness, then edema, pain, and finally decreased function. This sequence remains consistent regardless of the underlying cause of the inflammation, whether it be infection, injury, or other conditions. The timing of these symptoms can sometimes overlap, but their progression follows this predictable pattern. Understanding this sequence is essential for healthcare professionals to diagnose and manage inflammatory responses effectively. By recognizing these cardinal manifestations, nurses can provide targeted interventions to alleviate symptoms and promote healing..
Scene 14 (19m 45s)
[Audio] The inflammatory response is a complex physiological reaction involving multiple cell types, cytokines, as well as other mediators that work together to protect the body from injury or infection. When the body detects a pathogen or tissue damage, it initiates an inflammatory response to isolate the affected area, promote healing, and eliminate the threat. This response involves the activation of immune cells such as neutrophils and macrophages, which release chemical signals like cytokines and chemokines to recruit more immune cells to the site. The goal of this response is to restore homeostasis and prevent further damage. However, if the inflammatory response becomes chronic or dysregulated, it can lead to tissue damage and contribute to various diseases. Understanding the mechanisms of acute and chronic inflammation is crucial for developing effective treatments for conditions like arthritis, asthma, and cancer. By studying these processes, researchers can gain insights into how to modulate the immune system to prevent or manage disease..