Scene 1 (0s)
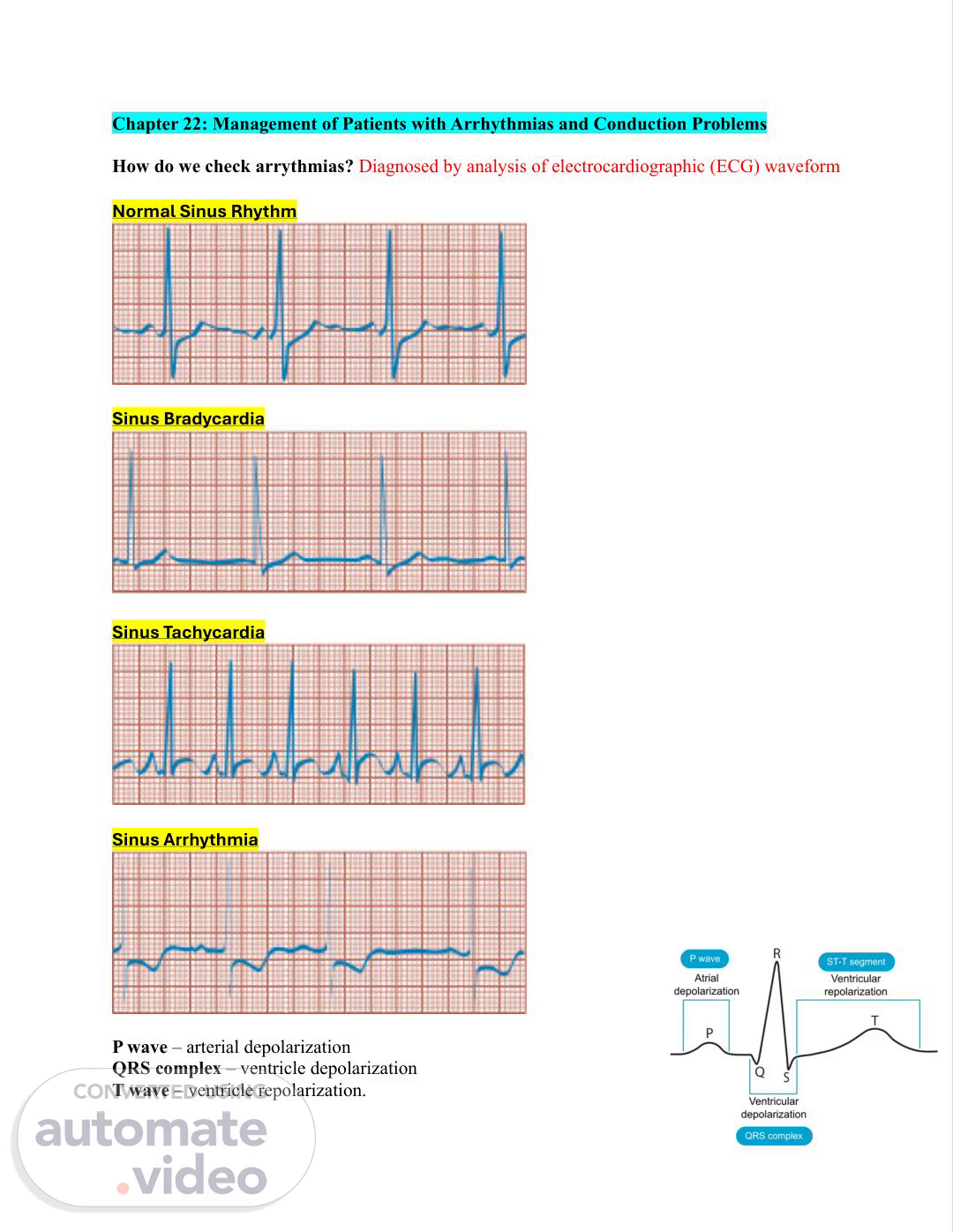
Chapter 22: Management of Patients with Arrhythmias and Conduction Problems How do we check arrythmias? Diagnosed by analysis of electrocardiographic (ECG) waveform Normal Sinus Rhythm Sinus Bradycardia Sinus Tachycardia Sinus Arrhythmia P wave – arterial depolarization QRS complex – ventricle depolarization T wave – ventricle repolarization..
Scene 2 (15s)
Types of Arrhythmias: • Atrial - Premature atrial complex - Atrial flutter - Atrial fibrillation • Ventricular - Premature ventricular complex: (they are stress induced) - Ventricular tachycardia - Ventricular fibrillation - Ventricular asystole The Electrocardiogram (ECG) • Skin Preparation (for proper adhesion & accurate results): o Abrade skin lightly with a clean, dry gauze pad to remove dead skin. o Clean area with soap and water to remove oils or lotions. o Clip excess hair (do not shave) if present at electrode site. o Hair interferes with electrode adhesion and causes artifacts (false signals/distorted results). Pacemakers • Used for slow heart rates (bradycardia), either temporary or permanent. • Indicated for symptomatic AV or ventricular conduction disorders. • May also be used to control certain tachyarrhythmias unresponsive to meds. • Electronic device that provides electrical stimuli to heart muscle • Types: o Permanent: after acute MI or during open heart surgery o Temporary: only in hospital settings Pacemaker Patient Education • Avoid high-output electrical generators – they can reprogram the pacemaker. • Most household electronics (e.g., microwaves) are safe with modern pacemakers. • Do not raise affected arm above shoulder for 1 week after pacemaker placement. • Walk quickly through antitheft alarms; avoid standing near them. o These alarms may trigger but usually do not interfere with pacemaker function. • Avoid strong electromagnetic fields, such as MRI machines. Complications of Pacemaker Use • Infection • Bleeding or hematoma formation • Dislocation of lead • Skeletal muscle or phrenic nerve stimulation • Cardiac tamponade • Pacemaker malfunction or battery failure • Psychosocial effects: Monitor patient for signs of isolation/depression, poor body image after pacemaker implantation..
Scene 3 (1m 15s)
Defibrillation • Used for pulseless clients only. • Indicated rhythms: o Ventricular fibrillation (V-fib) o Pulseless ventricular tachycardia (V-tach) • Epinephrine: o Give ASAP after first unsuccessful shock o Then every 3–5 minutes • Antiarrhythmics (e.g., amiodarone, lidocaine) are used if dysrhythmia continues. • Current delivery is unsynchronized Safety Measures for Defibrillation • Ensure good contact between skin, pads, and paddles. • Use a conductive medium and apply 20–25 pounds of pressure. • Position paddles to avoid contact with bedding, clothing, medication patches, or oxygen flow. • For defibrillation: Turn the synchronizer OFF. • For cardioversion: Turn the synchronizer ON. • Do not charge the device until ready to deliver the shock. • Call “clear” three times and perform safety checks before shocking. • Ensure no one is touching the patient, bed, or equipment during shock delivery. • Use an appropriate conducting agent (not water) between skin and paddles to prevent arcing (electrical shock). Cardioversion • Used for patients with a pulse and hemodynamic instability. • Turn the synchronizer ON. • Indicated rhythms: o Atrial fibrillation (AFib) o Atrial flutter o Supraventricular tachycardia (SVT) o Ventricular tachycardia (with a pulse) • Purpose: Restore normal sinus rhythm. • Current delivery is synchronized with the R wave on the ECG. o This minimizes risk of inducing arrhythmias by avoiding the vulnerable repolarization phase (T wave). Implantable Cardioverter Defibrillator (ICD) – For arrhythmias • Device detects and terminates life-threatening tachycardia and fibrillation (anti-tachycardia pacing). • Beneficial for patients who have survived sudden cardiac death. • Recommended for patients with CAD, 40 days post-acute MI, and moderate to severe left ventricular dysfunction. • Also indicated for patients with nonischemic dilated cardiomyopathy lasting at least 9 months. • After a permanent electronic device (pacemaker or ICD) is inserted, the client's heart rate and rhythm are monitored by ECG..
Scene 4 (2m 20s)
Nursing Management of the Patient with a Permanent Electronic Device • ECG assessment to monitor cardiac rhythm. • Chest X-ray (CXR): o Performed post-procedure and before discharge. o Confirms lead placement and rules out pneumothorax. Signs of Diminished CO • Syncope • Lightheadedness • Dizziness • Decreased BP • JVD • Pale and cool skin • Fatigue • Chest discomfort • Palpitations Chapter 23: Management of Patients with Coronary Vascular Disorders Angina Pectoris A clinical syndrome characterized by episodes of paroxysmal pain or pressure in the anterior chest caused by insufficient coronary blood flow, most often attributed to atherosclerosis • Stable angina: predictable and consistent pain occurring on exertion and relieved by rest and/or nitroglycerin. • Unstable angina: symptoms increase in frequency and severity; may not be relieved by rest or nitroglycerin. Factors that can cause Angina • Physical exertion (exercise) • Exposure to cold (causes vasoconstriction and increased BP) • Eating a heavy meal (reduced blood supply to heart muscle) • Stress or any emotion-provoking situation (increased BP, HR, and myocardial workload) Clinical Manifestations of Angina Pectoris • The most common manifestation of myocardial ischemia is the onset of chest pain. • Pain may be accompanied by severe anxiety and a sense of impending doom. • Typically felt deep behind the sternum (retrosternal). • May radiate to the neck, jaw, shoulders, and inner upper arms (usually left). • Diabetic patients feel minimal to no pain due to neuropathy, older adult feel weakness. Treatment for Angina Pectoris • Nitroglycerin o Pharmacologic Class: Nitrate o Therapeutic Class: Vasodilator o MOA: Improves blood flow to heart muscle and relieves pain; decrease myocardial O2 demand. Relaxes both arterial and venous smooth muscle; dilate coronary arteries. Reduce myocardial workload, lower myocardial oxygen demand..
Scene 5 (3m 24s)
• Antiplatelet/anticoagulation medication • Aspirin • Beta-Blockers • CCB Acute Coronary Syndrome (ACS) and Myocardial Infarction (MI) • ACS: an emergent situation characterized by an acute onset of myocardial ischemia that results in myocardial death (i.e., MI) if definitive interventions do not occur promptly. • The spectrum of ACS includes: Unstable angina, NSTEMI, STEMI. ACS Clinical Manifestations • Chest pain that occurs suddenly and continues despite rest and medication is the presenting symptom in most patients with ACS • The signs and symptoms of MI cannot be distinguished from those of unstable angina; hence, the evolution of the term acute coronary syndrome. Assessment and Diagnostic Findings of ACS • ECG changes o Elevation in the ST segment in two contiguous leads is a key diagnostic indicator for MI. • Lab studies o Cardiac enzymes o Troponin o Creatine kinase (CK) o Myoglobin. STEMI vs NSTEMI • STEMI: The patient has ECG evidence of acute MI with characteristic changes in two contiguous leads on a 12-lead ECG. (SEVERE DAMAGE TO MYOCARDIUM) • NSTEMI: The patient has elevated cardiac biomarkers (e.g., troponin) but no definite ECG evidence of acute MI. (LESS DAMAGE TO MYOCARDIUM) ACS Nursing Management • Goals of medical management are to minimize myocardial damage, preserve myocardial function, and prevent complications. • The patient with MI should receive: Oxygen, Aspirin, Nitroglycerin, and Morphine. o Morphine is the drug of choice to reduce pain and anxiety, and reduces preload and afterload, decreasing the work of the heart. o Oxygen and medication therapy o Frequent VS assessment o Continuous cardiac monitoring o Physical rest in bed with head of bed elevated (bed rest) o Relief of pain helps decrease workload of heart o Monitor I&O, kidney function, electrolytes and tissue perfusion o Frequent position changes to prevent respiratory complications o The use of ACE inhibitors in patients after MI decreases mortality rates. o A beta-blocker can also be used if arrhythmias occur. it should be introduced within 24hr.
Scene 6 (4m 29s)
Chapter 24: Management of Patients with Structural, Infectious, and Inflammatory Cardiac Disorders Types of Infectious Disease of the Heart Rheumatic endocarditis (diagnostic exam: echo) • Occurs most often in school-age children after group A beta-hemolytic streptococcal pharyngitis; need to promptly recognize and treat “strep” throat to prevent rheumatic fever Infective endocarditis (oral care) • Usually develops in people with prosthetic heart valves or structural cardiac defects; also occurs in patients who are IV drug abusers and in those with debilitating diseases, indwelling catheters, hemodialysis patients, or patients receiving prolonged IV therapy S/S of Infective Endocarditis Primary Symptoms: Fever & Heart Murmur Embolic and Immune-Related Manifestations • Petechiae: clusters seen on skin, conjunctiva, and mucous membranes • Osler nodes: small, painful nodules on fingers or toes • Janeway lesions: painless, flat red or purple macules on palms, soles, fingers, or toes • Roth spots: retinal hemorrhages with pale centers seen in the eye fundus • Splinter hemorrhages: reddish-brown streaks under fingernails or toenails Pericarditis • Inflammation of the pericardium; many causes; potential complications include pericardial effusion and cardiac tamponade (fluid accumulation) S/S of Pericarditis • May be asymptomatic • Most common symptom: chest pain o Can also occur below the clavicle, neck, or left scapular area o Pain worsens with deep inspiration, lying down, or turning • Classic finding: pericardial friction rub o Creaky or scratchy sound o Best heard at the left lower sternal border Other Symptoms • Fever • Increased WBC count • Anemia • Elevated ESR or CRP (inflammatory markers) • Nonproductive cough • Hiccups • Dyspnea and respiratory splinting • Tachycardia.
Scene 7 (5m 30s)
Myocarditis • An inflammatory process involving the myocardium; most common pathogens involved in myocarditis tend to be viral; in endocarditis, they tend to be bacterial; complications include cardiomyopathy and heart failure. S/S of Myocarditis • Common Symptoms: o Fatigue o Dyspnea (shortness of breath) o Syncope (fainting) • Palpitations • Occasional chest or upper abdominal discomfort • Often presents with flu-like symptoms • May lead to: CHF & Sudden cardiac death (know this) Infectious Diseases of the Heart: Diagnosis • Diagnostic tools: blood cultures, echocardiogram, CBC, rheumatoid factor, ESR, CRP, ECG, cardiac catheterization, TEE, CT scan. Infectious Diseases of the Heart: Prevention • Antibiotic prophylaxis before certain procedures • Ongoing oral hygiene (risk for bacteremia = infective endocarditis) • Female patients are advised NOT to use IUDs • Meticulous care should be taken in patients “at risk” who have catheters • Catheters should be removed as soon as they are no longer needed • Immunizations Valvular disorders • Regurgitation: The valve does not close properly, and blood backflows through the valve. • Stenosis: The valve does not open completely, and blood flow through the valve is reduced. • Valve prolapse: The stretching of the valve leaflet into the atrium during systole. Specific Valvular Disorders • Mitral valve prolapse • Mitral regurgitation: a condition in which blood flows from the left ventricle back into the left atrium during systole. • Mitral stenosis: results in reduced blood flow from the left atrium into the left ventricle. • Aortic regurgitation: backward flow of blood into the left ventricle from the aorta during diastole. • Aortic stenosis: narrowing of the orifice between the left ventricle and aorta. Valvular Heart Disorders: Nursing Management • Monitor for complications o Heart failure o Arrhythmias o Other symptoms: dizziness, syncope, angina pectoris.
Scene 8 (6m 35s)
Education: report new symptoms or changes in symptoms, educates the patient that an infectious pathogen, usually a bacterium, can adhere to a diseased heart valve more readily than to a normal valve resulting in endocarditis Chapter 25: Management of Patients with Complications from Heart Disease Heart Failure (HF) • Heart failure (HF) is a clinical syndrome resulting from structural or functional cardiac disorders that impair the ability of a ventricle to fill or eject blood; the heart is unable to pump enough blood to meet the body’s metabolic demands or needs Heart Failure Risk Factors • HF is more prevalent among African Americans and Hispanics. • The risk for having HF increases with advancing age. o For adults over 60 years of age, HF is more prevalent among men. • Coronary artery disease (CAD)/Atherosclerosis • Myocardial infarction (MI) • Hypertension • Cardiomyopathy • Valvular heart disease • Chronic kidney disease • Arrhythmias (e.g., atrial fibrillation) • Cigarette smoking • Obesity • Poorly managed diabetes • Metabolic syndrome Clinical Manifestations of Heart Failure Right Sided • Viscera and peripheral congestion • Jugular venous distention (JVD) • Dependent edema (lower edema) • Hepatomegaly • Ascites (fluid accumulation in abdomen) – paracentesis • Weight gain Left Sided • Pulmonary congestion, crackles • S3 or “ventricular gallop” • Dyspnea on exertion (DOE) • Low O2 sat • Dry, nonproductive cough initially • Oliguria o As cardiac output decreases and catecholamine levels rise, renal blood flow diminishes, leading to reduced urine output..
Scene 9 (7m 27s)
Pharmacological Therapy • Diuretics: decreases fluid volume, monitor serum electrolytes o Patients should take in the morning to avoid urination overnight o Examples: Furosemide, Hydrochlorothiazide, Spironolactone • Angiotensin-converting enzyme (ACE) inhibitors. o Examples: Lisinopril, enalapril • Angiotensin II receptor blockers (ARBs): o Examples: valsartan, losartan • Beta-blockers: prescribed in addition to ACE inhibitors; may be several weeks before effects seen; use with caution in patients with asthma or bronchospastic disease. • Digitalis (digoxin): improves cardiac contractility (positive ionotropic effect); monitor for digitalis toxicity especially if patient is hypokalemic and has visual disturbances. (monitor K) • IV medications: indicated for hospitalized patients admitted for acute decompensated HF. o Vasodilators: IV nitroglycerin, nitroprusside, nesiritide; enhance symptom relief. Contraindicated in hypotension, requires continues BP monitoring. Nursing Interventions • Manage fluid volume o Assess for symptoms of fluid overload (JVD, Edema, Ascites, Crackles) o Daily weight o I&O o Diuretic therapy; timing of meds o Fluid intake; fluid restriction o Maintenance of sodium restriction Pulmonary Edema (complication of HF) • Clinical manifestations: restlessness, anxiety, tachypnea, dyspnea, cool and clammy skin, cyanosis, weak and rapid pulse, cough, lung congestion (moist, noisy respirations), increased sputum production (sputum may be frothy and blood tinged), decreased level of consciousness Management of Pulmonary Edema/Nursing Interventions • Positioning: Sit patient upright with legs dependent (dangling) • Early recognition (monitor lung sounds and for signs of decreased activity tolerance and increased fluid retention) • Providing psychological support • Oxygen therapy (Start with a non-rebreather mask) • Medications (Monitor I&O) o Diuretics (furosemide) o Vasodilators (nitroglycerin).
Scene 10 (8m 27s)
Chapter 26: Assessment and Management of Patients with Vascular Disorders Peripheral Artery Disease (PAD) • Hallmark symptom is intermittent claudication described as aching, cramping, or inducing fatigue or weakness • Occurs with some degree of exercise or activity • Relieved with rest • Ischemic rest pain is usually worse at night and often wakes the patient • Placing extremity in dependent position reduces pain (have the feet dangling). Assessment finding of PAD • Nails may appear thickened and opaque. • Skin may be: o Shiny, atrophic, and dry o With sparse or absent hair • Gangrene may be present in advanced cases. • Assessment includes comparison of right and left extremities Risk Factors for Atherosclerosis and PAD Modifiable • Nicotine use • Diabetes • Hypertension • Hyperlipidemia • Diet • Stress • Sedentary lifestyle • C-reactive protein • Hyperhomocysteinemia o Common amino acid in the blood, mostly acquired from eating meat. High levels of it are linked to early development of heart disease. Non-modifiable • Increasing age • Familial predisposition/genetics Chapter 27: Assessment and Management of Patients with Hypertension Hypertension • Confirmation of diagnosis by average of two blood pressure readings Classification of BP for Adults 18 Years and Older • Normal Blood Pressure o Systolic <120 mm Hg and Diastolic <80 mm Hg • Elevated Blood Pressure o Systolic 120–129 mm Hg and Diastolic <80 mm Hg • Stage 1 hypertension o Systolic 130–139 mm Hg or Diastolic 80–89 mm Hg • Stage 2 hypertension o Systolic >140 mm Hg or Diastolic >90 mm Hg.
Scene 11 (9m 22s)
HTN: Clinical Manifestations • Usually, no symptoms other than elevated blood pressure • Symptoms related to organ damage are seen late and are serious o Retinal and other eye changes o Renal damage o Myocardial infarction o Cardiac hypertrophy o Stroke • Masked hypertension: patients exhibit high BP at levels consistent with HTN in settings outside the hospital/clinic, and BP is normal in health care settings o If untreated, pts can go on to experience adverse CV events (e.g., MI, strokes) and mortality • White coat hypertension: hypertensive blood pressure readings in the health care setting but are within normal ranges in other settings o Pts may receive treatment that is not warranted HTN: Medical Management • Goal is to prevent complications and death • Maintain blood pressure o <130/80 mm Hg • Lifestyle modifications o Weight reduction o DASH diet (decreased sodium intake diet) o Regular physical activity o Reduced alcohol consumption • Pharmacologic therapy o Decrease peripheral resistance, blood volume o Decrease strength and rate of myocardial contraction o Diuretics o Beta-blockers o Alpha1-blockers o Combined alpha- and beta-blockers o Vasodilators o ACE inhibitors o ARBs o Calcium channel blockers o Dihydropyridines o Direct renin inhibitors Hypertensive Crises • Hypertensive emergency o Blood pressure >180/120 mm Hg and must be lowered immediately to prevent further damage to target organs o Examples of target organ damage: hypertensive encephalopathy, ischemic stroke, MI, heart failure with pulmonary edema, dissecting aortic aneurysm, and renal failure. o Treatment: § IV vasodilators: sodium nitroprusside, nicardipine, fenoldopam mesylate, enalaprilat, nitroglycerin.
Scene 12 (10m 18s)
• Hypertensive urgency o Blood pressure >180/120 mm Hg in stable patients but no evidence of immediate or progressive target organ damage based on clinical exam and results of lab studies o Patients nonadherent to medication regimen o Treatment: § Fast-acting oral agents: • Beta-adrenergic blocker • Angiotensin-converting enzyme inhibitor • Alpha2-agonist Chapter 19: Management of Patients with Chest and Lower Respiratory Tract Disorders Atelectasis • Definition: A condition where the alveoli close or collapse, preventing proper gas exchange. • Assessment & Diagnosis: o Increased work of breathing and hypoxemia. o Decreased breath sounds and crackles over the affected area. • Expected finding: Pulse oximetry may demonstrate a low saturation of hemoglobin with oxygen less than 90%. • Diagnostic exam: Chest x-ray may suggest a diagnosis of atelectasis. Acute Atelectasis: • Acute atelectasis is the most common, especially in: o Postoperative patients, particularly after thoracic or upper abdominal surgeries. o Immobilized patients, due to shallow breathing or ineffective coughing. Acute Atelectasis Signs & Symptoms: • Pleural pain • Tachycardia • Tachypnea (marked respiratory distress may be present) • Central cyanosis (late sign of hypoxemia) • Orthopnea (difficulty breathing when supine) Chronic Atelectasis: • Predisposes the patient to pulmonary infections (S/S = fever, cough with sputum, SOB, crackles or diminished breath sounds) Chronic Atelectasis Signs & Symptoms: o Pleural pain o Pulmonary infection o Tachycardia o Tachypnea o Central cyanosis Atelectasis Prevention: First line measures: Frequent turning, early ambulation, lung volume expansion maneuvers and coughing..
Scene 13 (11m 14s)
o Frequent turning o Early mobilization/ambulation o Strategies to expand lungs and manage secretions o Incentive spirometer o Voluntary deep breathing/coughing o Secretion management o Pressurized metered-dose inhaler Pleural Effusion Definition: a collection of fluid in the pleural space, is rarely a primary disease process; it is usually secondary to other diseases such as heart failure, TB, pneumonia, pulmonary infections (particularly viral infections). Pleural Effusion Signs and Symptoms: • Fever (pneumonia) • Chills • Pleuritic pain • Dyspnea (malignant effusion) • Orthopnea • Cough Pleural Effusion Assessment and Diagnostic Findings: • Decreased or absent breath sounds; decreased fremitus; and a dull, flat sound on percussion. • Tracheal deviation away from the affected side may also be apparent (tension pneumothorax) o Pleurodesis: performed using thoracoscopic approach or chest tube for tension pneumothorax. Pleural Effusion Diagnosed by: • Physical examination • Chest x-ray • Chest CT • Thoracentesis (fluid analysis) confirm the presence of fluid. Acute Respiratory Failure (ARF) Definition: Sudden and life-threatening deterioration of the gas exchange function of the lungs Acute respiratory failure is defined as hypoxemia and hypercapnia with resp acidosis ARF Clinical Manifestations: • Early Signs: o Restlessness o Fatigue o Headache o Dyspnea o Tachycardia o HTN • Late Signs: o Confusion o Lethargy o Tachycardia o Tachypnea o Diaphoresis o Central Cyanosis o Respiratory arrest..
Scene 14 (12m 1s)
ARF Nursing Intervention to Enhancing Gas Exchange: • Judicious (wise) use of analgesics to relieve pain without suppressing respiratory drive. o No Morphine (causes respiratory depression) • Frequent repositioning to diminish the pulmonary effects of immobility. ARF Nursing Intervention to Promote Effective Airway Clearance: • Assess lung sounds at least every 2 to 4 hours • Measures to clear airway: suctioning, CPT, position changes, promote increased mobility • Humidification of airway Administer medications: • Bronchodilators o Short acting Beta 2-Agonist: § Albuterol § Levalbuterol o Long-Acting Beta 2-Agonist: § Salmeterol § Formoterol o Anticholinergics § Ipratropium (short-acting) § Tiotropium (long-acting) o Methylxanthines § Theophylline • Mucolytics o Acetylcysteine o Guaifenesin Chapter 20: Management of Patients with Chronic Pulmonary Disease Chronic obstructive pulmonary disease (COPD) • Chronic obstructive pulmonary disease (COPD) is a slowly progressive respiratory disease of airflow obstruction. • Preventable and treatable but not fully reversible COPD Pathophysiology: • Airflow limitation in chronic respiratory conditions is progressive and stems from an abnormal inflammatory response to harmful particles or gases. This chronic inflammation leads to tissue damage and the formation of scar tissue, which contributes to: o Narrowing of the airways o Reduced lung elasticity due to scarring in the parenchyma (compliance) o Thickening of pulmonary blood vessels and smooth muscle hypertrophy, resulting in pulmonary hypertension. COPD Clinical Manifestations • Three primary symptoms: o Chronic cough o Sputum production o Dyspnea § Weight loss due to dyspnea and increased work of breathing • Barrel Chest.