Scene 1 (0s)
Dental CARIES.
Scene 2 (6s)
Reading Materials: Pinkham and avery’s. Pediatric Dentistry. Elsevier Saunders 2005. pp. 200-204 Handbook of Dental Hygienist” – Handbook of BSc level Dental Hygienist Program. pp. 40-44.
Scene 3 (19s)
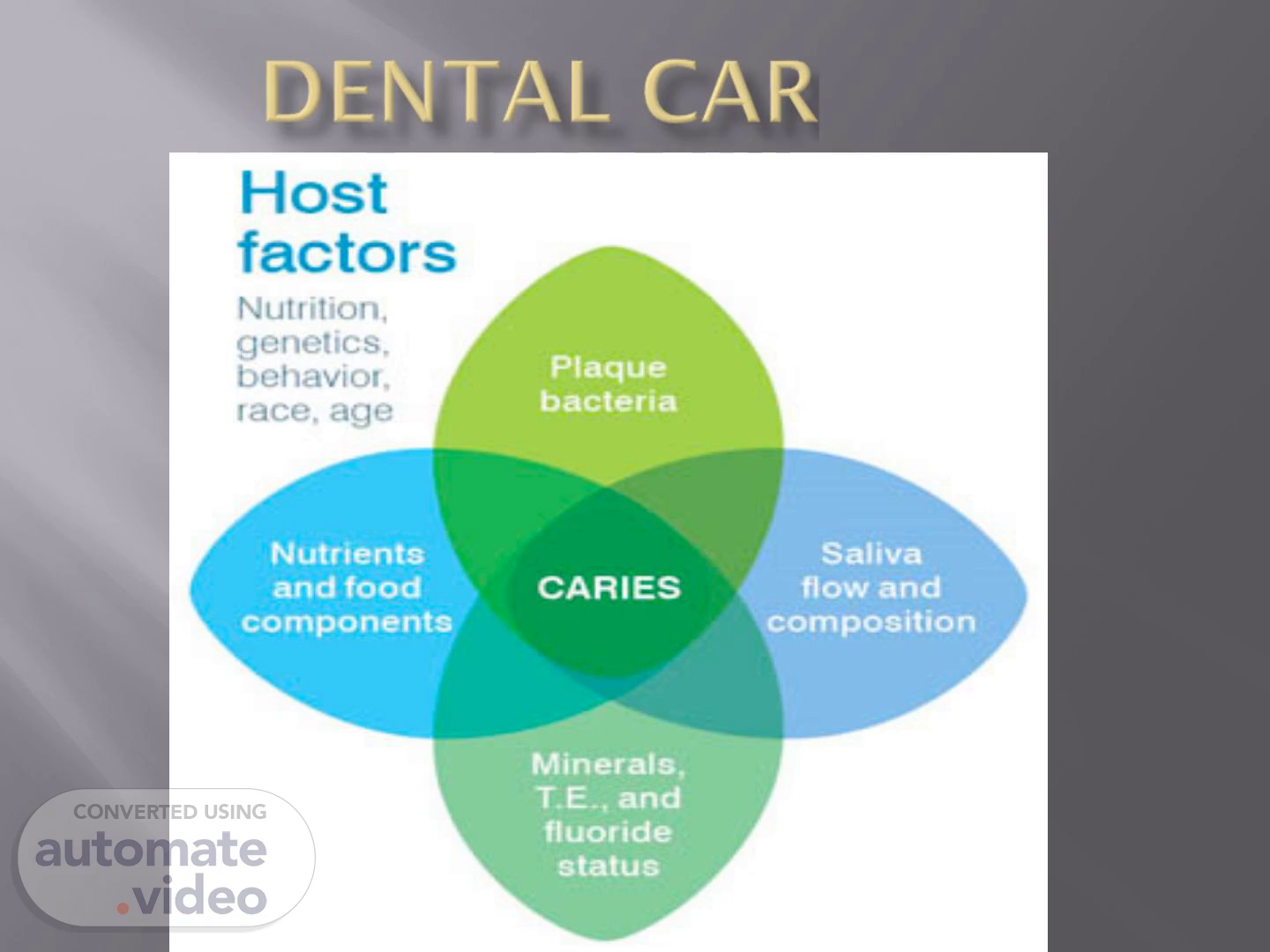
Etiology of dental caries. What is caries??? Caries is an infectious and communicable disease and multiple factors influence the initiation and progression of the disease..
Scene 4 (30s)
The disease is recognized to require. (1)a susceptible tooth; (2) presence of bacteria; (3) access to refined, fermentable carbohydrate; (4) time..
Scene 5 (39s)
[image] ACID BACTERIA SUGARS dam TOOTH SURFACES Over time, this process can cause a hole..
Scene 6 (46s)
Dental caries is a dietary carbohydrate modified infectious disease in which saliva functions as a critical regulator. In this definition, the term "infectious" is used in its most basic sense, meaning colonization of the oral cavity by bacteria..
Scene 7 (1m 0s)
Dental caries is a disease of the dental hard tissues characterized initially by the decalcification of the inorganic portions of the tooth. Loss of the mineral content is then followed by breakdown of the organic matrix. This destructive process results from the metabolism of refined carbohydrates by oral microorganisms..
Scene 8 (1m 19s)
Cariogenic bacteria. The seven species of Streptococcus associated with dental caries are collectively known as the "mutans streptococci." All are members of the S. viridans group. They are currently presumed to have the major role in the initiation of the lesion, even though they are not the first to colonize the tooth surface. Increasing attention in recent cariology research is being given to the relative cariogenic potential of various combinations of plaque bacteria,including some strains of Actinomyces..
Scene 9 (1m 42s)
Cariogenic bacteria possess three properties that enable them to function in the disease process..
Scene 10 (1m 55s)
Mutans streptococci. Mutans streptococci have only a weak ability to colonize the oral cavity, and they require a hard, non-desquamating surface, such as teeth, for colonization. Because their ecological niche is on the tooth surface, mutans streptococci were not found in the mouths of infants until the later stages of primary tooth eruption. It was shown that mouth-to-mouth transmission of mutans streptococci takes place between mothers and their children..
Scene 11 (2m 17s)
Transmission may occur in two ways. Direct transmission involves the comingling of the parent's and child's saliva, as during kissing. Indirect transmission involves the placement of objects (spoon, pacifier, infant's fingers) into the parent's mouth, then into the infant's mouth..
Scene 12 (2m 32s)
Factors associated with colonization. Noncolonization.
Scene 13 (2m 46s)
[image].
Scene 14 (2m 51s)
Pellicle. The pellicle is approximately 1 micron in thickness, It is a clear, translucent layer, which may be stained by disclosing agents, nicotine, caffeine, etc., becomes brown, greyish or other colour..
Scene 15 (3m 8s)
Formation of pellicle. Within minutes after complete cleansing of the solid surface, a pellicle forms from protein and glycoprotein of saliva. The first colonisers adhere to the tooth surface initially through weak, reversible adhesion via van der Waals forces and they are removable by waterjet..
Scene 17 (3m 30s)
Dental biofilm(dental plaque). A biofilm is a complex microbial ecosystem formed by colonies of one or more different species attached to the tooth surface. The oral biofilm is a soft, non-mineralised, acquired, gel-like deposit attached to the tooth surfaces, restorations and implants via the pellicle..
Scene 18 (3m 46s)
Formation of Plaque. The initial bacterial colonization of teeth probably begins with organisms other than mutans streptococci, which do not have great ability to adhere to teeth. The mechanisms of initial colonization include (1) adherence of bacteria to pellicle or the enamel surface; (2) adhesion between bacteria of the same or different species; (3) subsequent growth of bacteria from small enamel defects and from cells initially attached to tooth structure..
Scene 20 (4m 12s)
Plaque development continues with the formation of extracellular polymer chains via the breakdown of sucrose into its two main components, glucose and fructose . The polymers are synthesized from each of these components. Chains of glucose and fructose, termed glucans and fructans, respectively, are sticky, gelatinous substances that further enhance the bacteria's ability to adhere to the tooth and to each other. Glucans and fructans also affect the rate at which saliva can enter the plaque to buffer the acid and reverse the demineralization process. Intracellular metabolism of carbohydrates leads to the production of acids, chiefly lactic, that can depress plaque pH from a resting level of about 6 to a value of 4 within minutes of contact with a fermentable carbohydrate..
Scene 21 (4m 43s)
Biofilm bacteria embedded within a matrix of extracellular polysaccharides are more than 1,000 times less sensitive to antimicrobials (e. g.,antibiotics) than free-floating (“planktonic”) bacteria.
Scene 23 (5m 3s)
The subgingival plaque formed from the supragingival biofilms grows into the sulcus.
Scene 24 (5m 15s)
[image].
Scene 25 (5m 20s)
Remineralization and demineralization. The process appears to be a dynamic one, involving both the loss of enamel mineral content and its replacement, with surface enamel functioning as a diffusion matrix. Enamel matrix provides relatively large channels through which acids, minerals, fluoride, and other ions may pass in both directions. Under normal oral conditions, equilibrium is established between mineral loss and mineral gain..
Scene 26 (5m 40s)
[image].
Scene 27 (5m 45s)
The balance can be disturbed, however, by environmental factors in the oral cavity, such as plaque fluid pH and the presence or absence of fluoride..
Scene 28 (6m 6s)
[image].
Scene 29 (6m 11s)
The presence of fluoride in the oral environment, even in very low concentration, can affect the equilibrium of this process in the opposite manner, leading to remineralization. This fluoride may come from the saliva, the plaque fluid, or from the demineralized enamel itself. During remineralization, fluoride facilitates the diffusion of calcium and phosphorus back into the lesion where partially dissolved hydroxyapatite crystals are rebuilt into fluoridated hydroxyapatite..
Scene 30 (6m 32s)
The flow, dilution, buffering, and remineralizing capacity of saliva are recognized to be critical factors that affect, and in some ways regulate, the progression and regression of the disease..
Scene 31 (6m 58s)
Causes of demineralization The critical pH for dissolution of enamel has been shown to be about 5.5..
Scene 33 (7m 42s)
Enamel lesion in case of white spot. [image].
Scene 34 (7m 49s)
Which factors decrease and increase the rate of remineralisation.
Scene 36 (8m 15s)
What is caries called“arrested leasion”. Even after cavitation of tooth occurs, if the pulp is not yet involved and if the cavitated area is open enough to be self-cleansing (plaque-free), the caries process can halt and become an “arrested lesion.” Arrested lesions typically exhibit much coronal destruction. The remaining exposed dentin is hard and usually very dark. There is no evidence of pulpal damage, and the patient has no pain..
Scene 39 (8m 53s)
What is rampant dental caries. Rampant caries has been defined as a suddenly appearing, widespread, rapidly burrowing type of caries, resulting in early involvement of the pulp and affecting those teeth usually regarded as immune to ordinary decay..
Scene 40 (9m 7s)
Which factors enhance the appearance of rampant caries.
Scene 43 (10m 2s)
What is severe early childhood caries or baby bottle tooth decay.
Scene 45 (10m 49s)
The American Academy of Pediatric Dentistry recommends.