Dementia Training - Module 1 - Part 9 - Stroke and Brain Injuries
Scene 1 (0s)
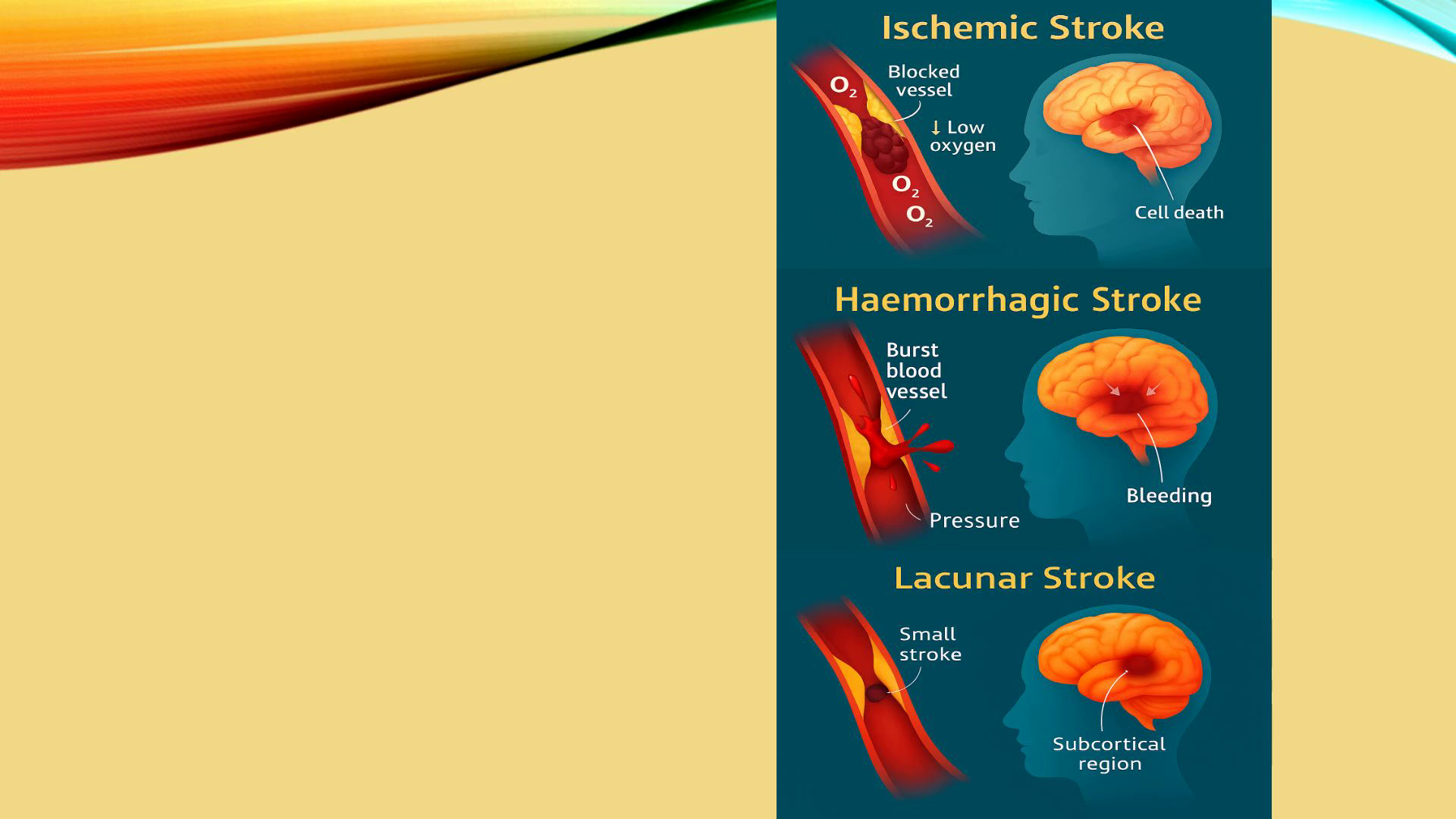
[Virtual Presenter] This is Part 9 of Module 1—a closer look at strokes and brain injuries and the effect they have on the brain and dementia. Ischemic strokes represent the most prevalent category of stroke. They occur when a blood vessel supplying the brain becomes obstructed, often due to a blood clot or the accumulation of fatty deposits. If this obstruction is not addressed promptly, it can lead to oxygen deprivation, resulting in the death of brain cells and subsequent cognitive decline. Haemorrhagic strokes arise from the rupture of a blood vessel, causing bleeding within or surrounding the brain. The pressure generated by this bleeding can damage brain cells and disrupt their normal functioning. Haemorrhagic strokes are often severe and are associated with an elevated risk of developing dementia. Lacunar strokes are characterised as small strokes that occur deep within the brain and affect tiny blood vessels. While each lacunar stroke may result in minor damage, the occurrence of multiple strokes can lead to substantial cognitive impairment. The presence of numerous lacunar strokes is linked to subcortical vascular dementia, a condition defined by executive dysfunction, alterations in mood, and progressive cognitive decline. The connection between stroke and dementia can feel overwhelming, especially since even a single stroke can increase the likelihood of developing dementia. For those who have experienced multiple strokes, the cumulative effects can be even more daunting. This underscores the importance of preventive measures to support cognitive health. The journey after a stroke is unique to each person. It can be influenced by factors such as the type, severity, and location of the stroke, as well as individual health conditions. Many individuals may find themselves facing post stroke cognitive impairment, which can bring challenges in areas like memory, attention, language, and executive function. If these difficulties continue for more than six months, they may be diagnosed as post stroke dementia,which can be challenging to accept. However, it’s important to remember that the brain has a remarkable ability to recover through a process called neuroplasticity. Engaging in rehabilitation and cognitive therapies can be incredibly beneficial, offering hope and support in reducing the risk of dementia after a stroke. Recovery can vary widely based on the specifics of the stroke and individual choices, but every small step counts. By understanding these pathways and the challenges they face, professionals and caregivers can provide compassionate support, helping individuals navigate their recovery journeys and work to preserve cognitive health. Your strength and resilience during this time are truly admirable..
Scene 2 (2m 58s)
[Audio] Another common type of secondary dementia is Traumatic Brain Injury (TBI), which can be a challenging and distressing condition. Traumatic brain injury occurs when an external force causes harm to the brain. These injuries can result from various incidents, such as falls, car accidents, sports impacts, or even assaults. Any event that leads to the brain moving suddenly within the skull. It's important to acknowledge that the severity of TBIs can vary significantly, with some individuals experiencing mild concussions while others face severe, life-altering injuries. Understanding the impact of such injuries is crucial for providing support and care to those affected. It's essential to understand how specific biological processes can affect our brain health after experiencing a traumatic brain injury (TBI). The buildup of abnormal tau protein and ongoing neuroinflammation can create a link between TBIs and dementia. This connection sheds light on the increased risk of dementia following such injuries. While it's reassuring to know that a single mild concussion may not dramatically raise this risk, many athletes face the reality of repeated mild TBIs in contact sports. These can accumulate over time, leading to significant damage. This situation highlights the urgent need for prevention, protective measures, and early intervention to safeguard everyone's well-being..
Scene 3 (4m 27s)
[Audio] Severe traumatic brain injuries (TBIs) can profoundly impact individuals, often leading to significant brain damage and an increased risk of developing dementia later in life. One such concern is Chronic Traumatic Encephalopathy (CTE), a specific form of dementia that arises from the repeated TBIs experienced by some athletes in contact sports like football, boxing, rugby, and hockey. CTE is characterised by abnormal tau protein deposits in the brain, which can cause distressing symptoms such as memory loss, cognitive decline, mood changes, and behavioural disturbances. It's essential to recognise that after a TBI, the journey doesn't end with the initial injury. A cascade of damaging events can continue for months or even years, contributing to further brain cell death. This ongoing damage serves as a reminder of the necessity for long-term monitoring and support, ensuring that those affected can receive the care they need and deserve. The brain, unfortunately, has a limited capacity for self-repair, which can make recovery from a traumatic brain injury (TBI) especially challenging. When someone experiences a TBI, it can set off a chain reaction of neurodegeneration that may continue long after the initial injury seems to have healed. This can lead to persistent brain inflammation, which can release harmful chemicals that further damage brain cells. It's essential to recognise that chronic inflammation is a common issue in many neurodegenerative conditions, including Alzheimer's disease, and this can be a source of anxiety for those affected and their families. Additionally, a TBI can disrupt the precious connections between neurons. When these communication pathways are damaged, it can result in difficulties with cognitive function, affecting daily life in significant ways. Repeated injuries may further reduce the brain's plasticity, its remarkable ability to adapt and reorganise itself, making the journey to recovery even more difficult. It's crucial to approach this situation with understanding and support for those navigating the complexities of brain health. In summary, we know that traumatic brain injuries (TBIs) can pose a significant risk for developing dementia. This is often due to the direct damage they inflict, the cumulative effects of repeated injuries, and the ongoing processes of inflammation and neurodegeneration that can follow. It's important to understand these factors, as this knowledge can empower us to prevent dementia and provide better support for those who have experienced brain injuries. Early intervention, rehabilitation, and compassionate management are critical in this journey. By addressing menopause-related changes, strokes, and brain injuries promptly, we can significantly reduce the risk of dementia and improve long-term outcomes for individuals and their families. Together, we can navigate these challenges and foster hope for a brighter future. In Part 10, we can summarise Module 1 before you complete the assessments..